The complex ecosystem of bacteria living in our digestive tracts, known as the gut microbiome, exerts a profound influence on our overall health. It is particularly significant in the context of food intolerance, where the interplay between gut bacteria and dietary components can either contribute to or alleviate uncomfortable symptoms. This article will delve into the mechanisms by which the gut microbiome affects food intolerance, and discuss strategies to harness the microbiome for better digestive health.
The Gut Microbiome: A Primer
Our gut microbiome is comprised of trillions of microorganisms, including bacteria, viruses, fungi, and protozoa. These microbial inhabitants are not mere passengers; they perform critical functions such as aiding digestion, synthesizing vitamins, and training the immune system. Each individual’s microbiome is unique, influenced by factors like genetics, diet, and environment.
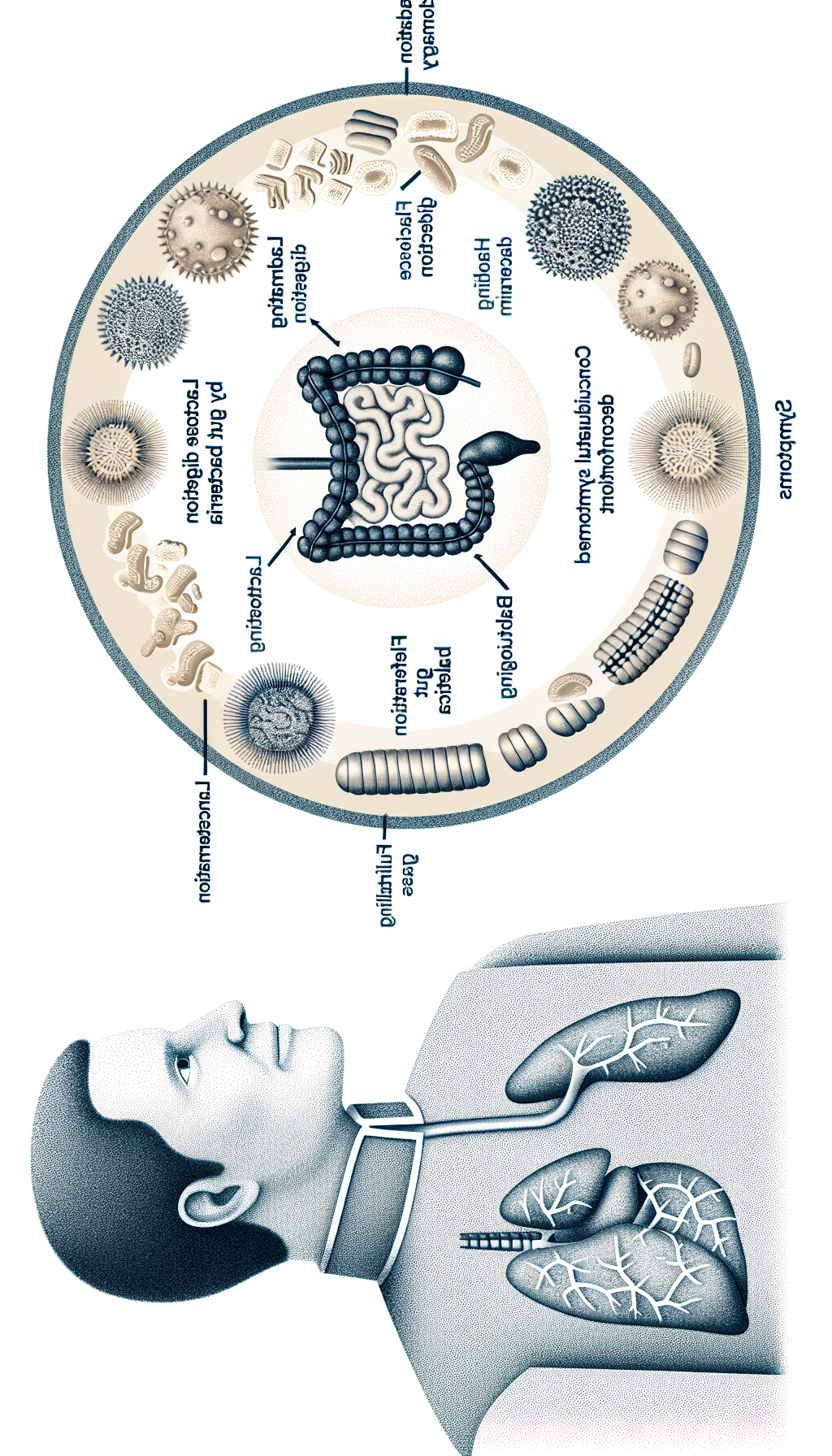
Recent research has illuminated the gut microbiome’s role in food intolerance, a condition characterized by difficulty digesting certain foods, leading to symptoms such as bloating, gas, and abdominal pain. Unlike food allergies, which involve the immune system’s overreaction to food proteins, food intolerances often stem from the lack of specific enzymes needed to break down food components, or from interactions between food and gut bacteria.
For a comprehensive understanding of digestive health and its relation to the gut microbiome, visit Avix Health’s section on Digestive Health.
Microbiome Imbalances and Food Intolerance
An imbalance in the gut microbiome, known as dysbiosis, can be a key contributor to food intolerance. Several factors can lead to dysbiosis, including antibiotic use, stress, and dietary choices. This imbalance can result in decreased microbial diversity and the overgrowth of certain bacteria that may exacerbate intolerance symptoms.
For example, some individuals may experience lactose intolerance due to a deficiency in lactase, the enzyme required to digest lactose. The undigested lactose then becomes food for gut bacteria, which ferment it, producing gas and causing discomfort.
To deepen your understanding of how diet influences the gut, consider reading about the role of plant-based diets in managing gastrointestinal disorders.
The Role of Bacteria in Digesting Problematic Foods
Some gut bacteria possess the ability to break down food components that the human digestive system cannot. These bacteria can be viewed as allies in combating food intolerance. For instance, certain strains are adept at breaking down complex carbohydrates and fibers, thereby reducing gaseous byproducts and discomfort.
Moreover, the gut microbiome can influence the gut’s permeability. A healthy microbiome contributes to a strong intestinal barrier, which is crucial in preventing undigested food particles from triggering inflammatory responses that can lead to intolerance symptoms.
For insights into maintaining a robust gut barrier, explore how dietary fibers affect intestinal barrier function.
Strategies to Modify the Microbiome for Better Food Tolerance
Adjusting the gut microbiome composition can be instrumental in addressing food intolerances. Here are some strategies:
Probiotic and Prebiotic Supplementation
Probiotics are live microorganisms that can confer a health benefit, while prebiotics are dietary fibers that feed beneficial gut bacteria. Supplementation with probiotics and prebiotics can help replenish and nurture a healthy microbiome, potentially improving tolerance to certain foods.
For the latest findings on probiotic supplementation, visit advancements in probiotic supplementation for gut health repair.
Diversify Your Diet
A varied diet rich in fruits, vegetables, and whole grains provides a wide range of substrates for different bacterial species, promoting a diverse and resilient microbiome.
Lifestyle Modifications
Stress management and regular exercise have been shown to have a positive impact on the gut microbiome. These lifestyle changes can support a healthy microbial balance and, in turn, improve food tolerance.
For further reading on the relationship between exercise and digestive function, see the impact of moderate exercise on digestive function.
The Future of Microbiome Research and Food Intolerance
Research into the gut microbiome is rapidly evolving, with new discoveries frequently emerging. One promising area of study is the development of microbiome-based diagnostics that can predict individual responses to different foods, paving the way for personalized nutrition plans to combat food intolerances.
External Resources for Further Exploration
- The International Scientific Association for Probiotics and Prebiotics provides updates on the latest research and guidelines on probiotics and prebiotics.
- The American Gastroenterological Association offers resources on digestive health, including the management of food intolerances.
- Monash University’s FODMAP Research provides cutting-edge insights into how certain foods affect those with IBS and related food intolerances.
- The Gut Microbiota for Health Expert Exchange platform by the European Society of Neurogastroenterology & Motility shares scientific developments related to gut health.
- The Food Intolerance Institute of Australia provides a wealth of information on food intolerance, including identification and management strategies.
In conclusion, the gut microbiome plays a critical role in food intolerance, but by understanding and nurturing this complex inner ecosystem, individuals can take meaningful steps towards improving their digestive comfort and overall health. As research continues to unravel the intricacies of the gut microbiome, the potential for new and effective interventions for food intolerance looks promising.