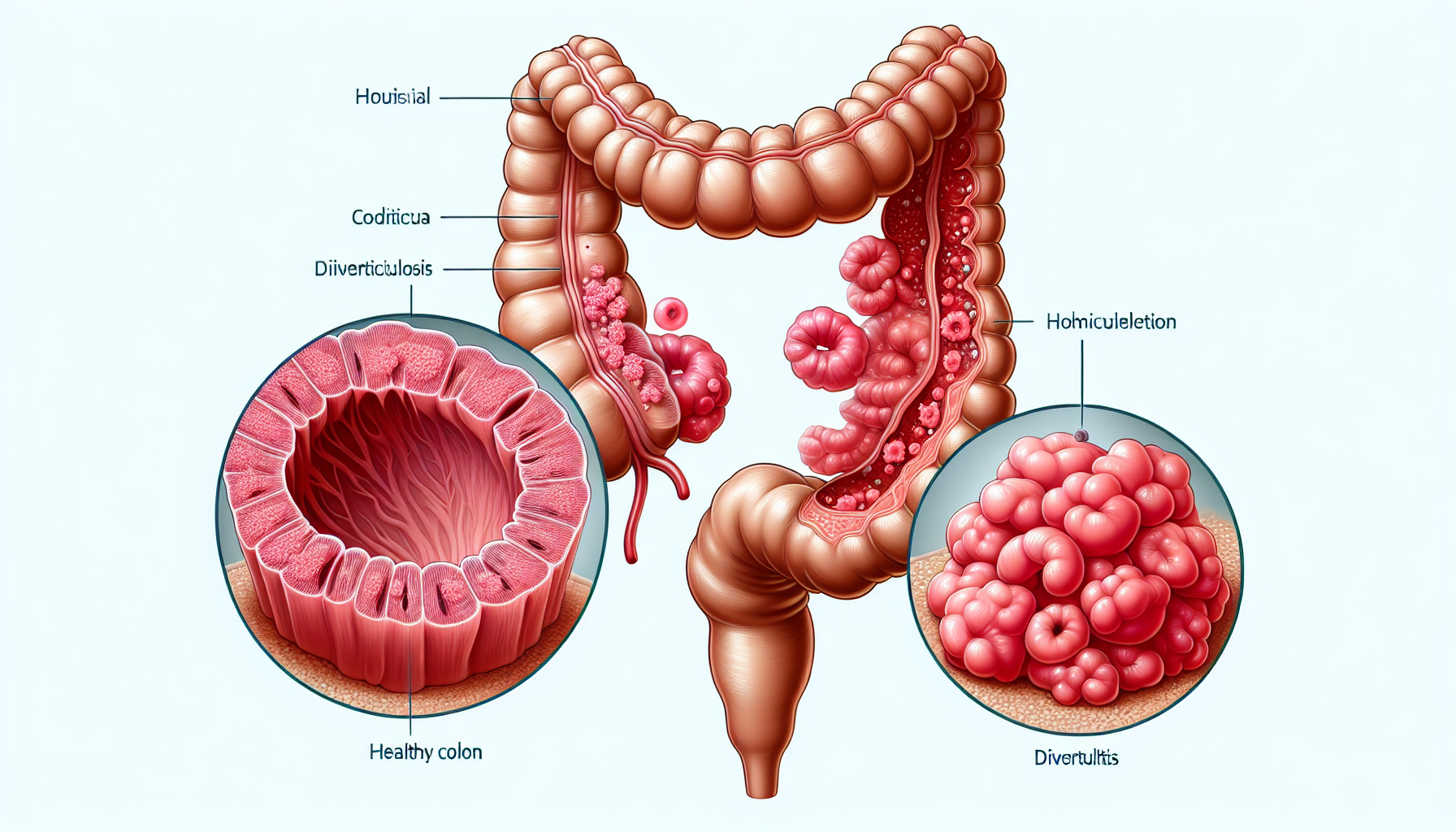
Diverticular disease is a common digestive condition that affects the large intestine, or colon. It typically manifests through the development of small, bulging pouches called diverticula in the lining of the digestive system. These pouches can cause a range of symptoms and complications, leading to two main conditions: diverticulosis and diverticulitis. This comprehensive article delves into the complexities of diverticular disease, exploring its symptoms, causes, management strategies, and the connection between overall digestive health and this condition.
What is Diverticular Disease?
Diverticular disease encompasses two related gastrointestinal conditions: diverticulosis, which is the presence of diverticula, and diverticulitis, which is the inflammation or infection of these pouches. Diverticulosis is often asymptomatic, but when symptoms do appear, they can include mild cramps, bloating, and constipation. Diverticulitis, on the other hand, can cause significant pain, fever, and digestive upset, and may require medical intervention.
The Role of Fiber and Diet
Diet plays a crucial role in the development and management of diverticular disease. A diet low in fiber is widely recognized as a contributing factor to the formation of diverticula. Fiber helps to soften the stool and decrease colon pressure, thus reducing the risk of diverticula forming. Incorporating a high-fiber diet is often recommended as a preventive measure and for those with diverticulosis to help manage the condition. For more information on the importance of fiber in digestive health, consider exploring the benefits of a high-fiber diet.
Symptoms and Diagnosis
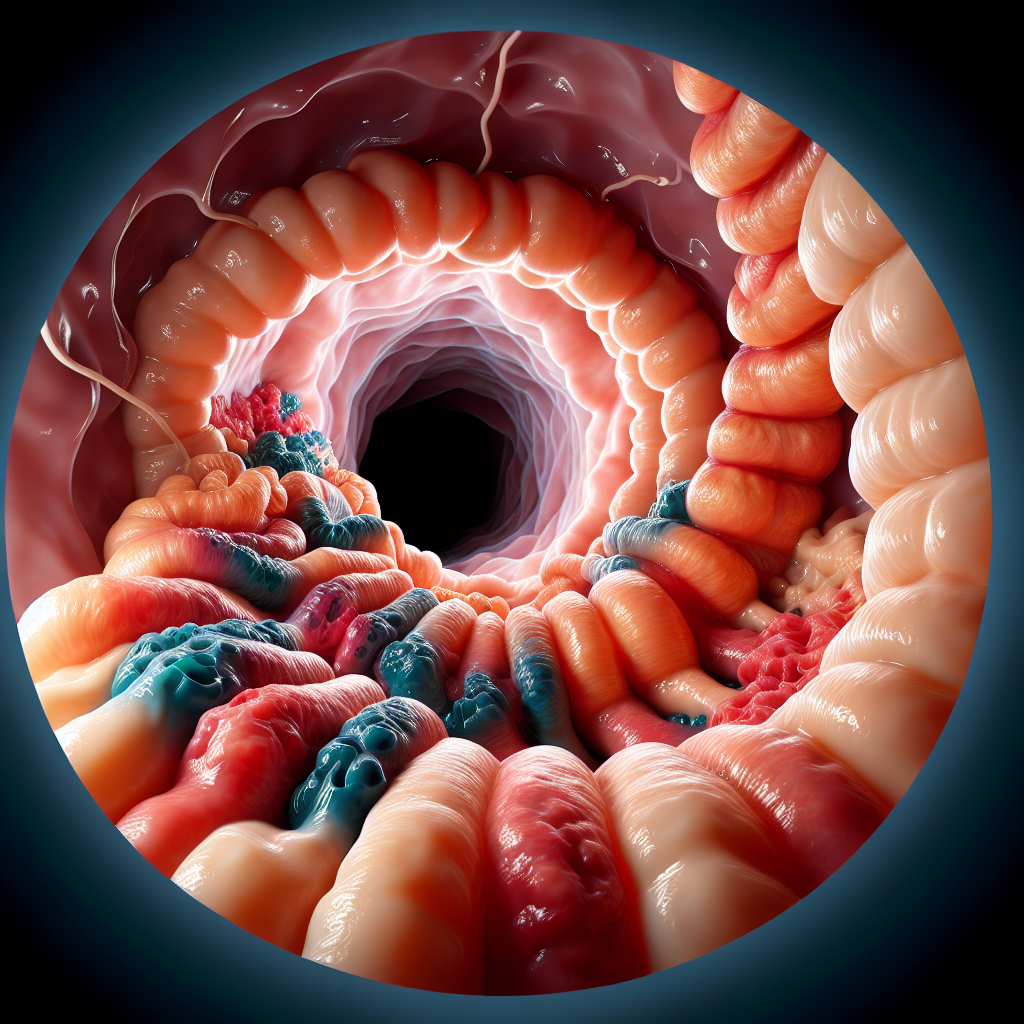
While diverticulosis might not cause symptoms, the progression to diverticulitis can lead to more noticeable signs. Symptoms of diverticulitis can include severe abdominal pain, usually on the left side, fever, nausea, and a marked change in bowel habits. Diagnosis typically involves a physical examination, and may include a CT scan or colonoscopy for confirmation.
Managing Diverticular Disease
The management of diverticular disease often involves dietary changes, antibiotics, and possibly surgery for severe cases of diverticulitis. Increasing the intake of dietary fiber can be beneficial, as well as avoiding foods that may irritate the colon, such as nuts and seeds, although recent studies have begun to question this advice.
For more comprehensive lifestyle strategies to enhance digestive health, including managing diverticular disease, readers may find value in exploring articles such as Strategies to Enhance Gut Flora and Promote Digestive Balance, which provides insights into maintaining a healthy gut environment.
Treatment of Diverticulitis
When diverticulitis occurs, treatment aims to reduce inflammation and prevent complications. Antibiotics are commonly prescribed, and in some cases, hospitalization may be necessary to manage severe infections or complications. If recurrent episodes occur or complications such as abscesses or fistulas develop, surgery may be required to remove the affected portion of the colon.
Prevention Strategies
Preventive measures for diverticular disease focus primarily on dietary and lifestyle modifications. Regular exercise, adequate fluid intake, and a diet rich in fruits, vegetables, and whole grains are recommended. Additionally, managing body weight and avoiding smoking are also suggested to reduce the risk.
Understanding the connection between overall health and the risk of diverticular disease is essential. For instance, the Impact of Sleep Patterns on Digestive Health highlights the importance of sleep in maintaining digestive system balance, which can influence the development and management of diverticular disease.
Complications and Risks
Complications from diverticular disease can be serious, including peritonitis, abscesses, and fistulas. Risk factors for developing diverticular disease include aging, a diet low in fiber, physical inactivity, obesity, smoking, and the use of certain medications like NSAIDs and steroids.
To gain insight into the connection between cholesterol levels and digestive health, which may also play a role in the development of diverticular disease, reading about The Connection Between Cholesterol Levels and Digestive Health can be enlightening.
Additional Resources
For those seeking more detailed information on diverticular disease and its management, there are several niche resources available:
- The Mayo Clinic offers an in-depth look at symptoms, causes, and treatments.
- The American Society of Colon and Rectal Surgeons provides valuable resources on disease management and surgical options.
- NutritionFacts.org explores the impact of diet, particularly plant-based diets, on diverticular disease.
These resources can provide additional support and information for individuals dealing with diverticular disease.
Conclusion
Diverticular disease is a common condition that can significantly impact one’s quality of life. Understanding its complexities, including the role of diet, symptoms, management strategies, and the importance of overall digestive health, is key to effectively addressing this condition. By making informed lifestyle choices and seeking appropriate medical care, individuals can manage the symptoms of diverticular disease and reduce the risk of complications.