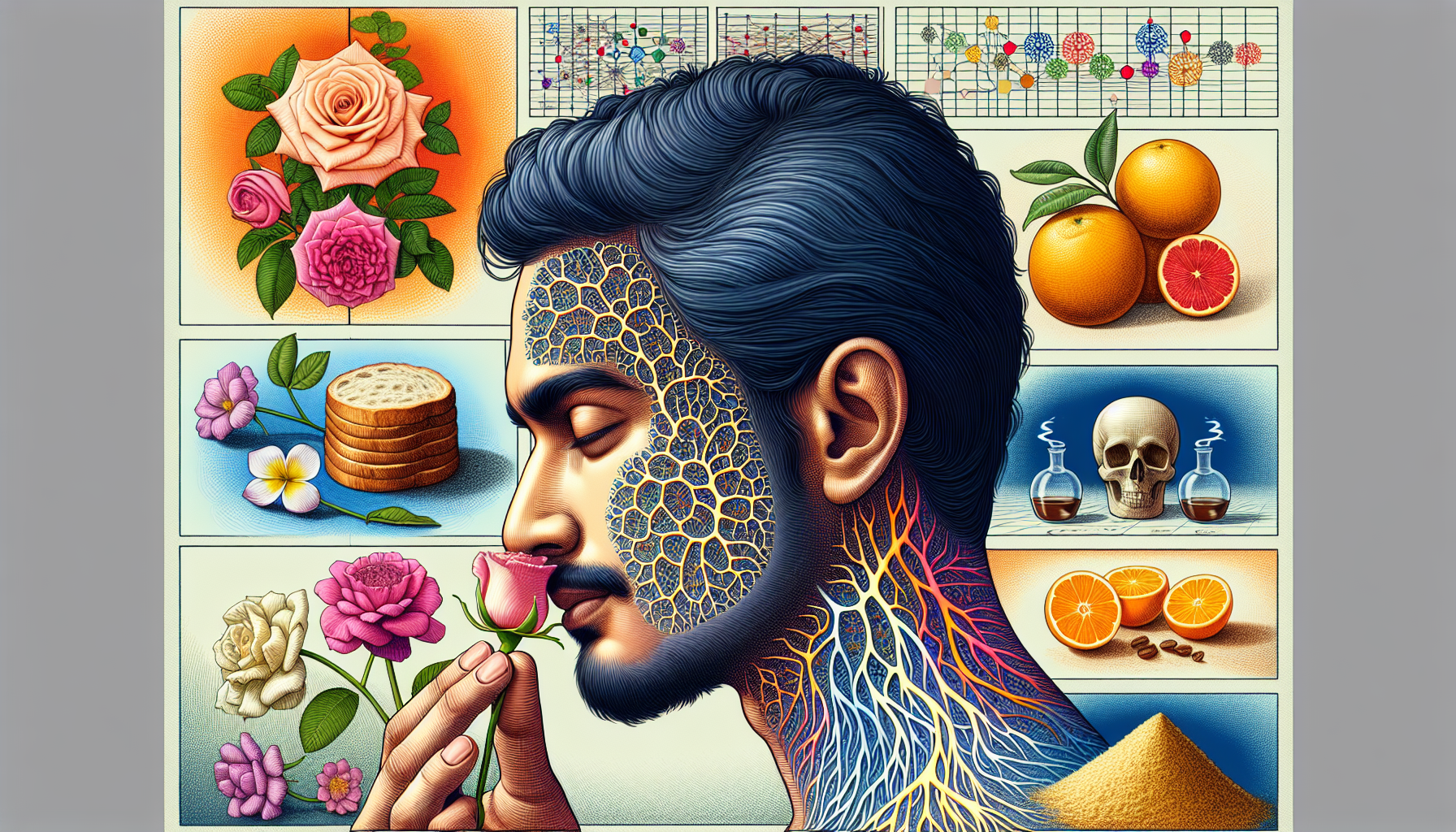
Olfactory processing disorders can profoundly affect an individual’s quality of life, influencing everything from personal safety to nutritional choices and social interactions. These disorders involve a disruption in the ability to recognize, interpret, and respond to smells. This comprehensive article aims to delve into the nature of olfactory processing disorders, their impacts, and the strategies for effective management and treatment.
What Are Olfactory Processing Disorders?
Olfactory processing disorders fall under the broader category of sensory processing issues, where the brain has trouble receiving and responding to information that comes in through the senses. Specifically, these disorders may manifest as an impaired ability to identify, differentiate, or appreciate various odors. The range of olfactory issues can span from anosmia, the complete loss of smell, to hyposmia, a reduced ability to smell, to more complex conditions where odors are misinterpreted or cause undue distress.
The sense of smell is closely linked with other vital functions, as it can trigger memories, influence emotional states, and even play a role in warning of dangers such as fire or spoiled food. Thus, disruptions in olfactory processing are not merely inconveniences; they can have significant ramifications for an individual’s health and well-being.
Causes and Diagnosis
Olfactory processing disorders can arise from a variety of causes, including head injuries, infections, neurological disorders, and congenital conditions. Sometimes, they may be a symptom of larger sensory processing disorders that affect multiple senses. To diagnose these conditions, healthcare professionals may employ a combination of patient history, physical examinations, and specialized tests that measure olfactory function.
For a more detailed understanding of sensory health and related conditions, the Sensory Health section on Avix Health provides valuable insights.
Impact on Daily Life
The inability to perceive odors properly can lead to challenges in personal hygiene, food enjoyment, and detection of environmental hazards. Moreover, olfactory disorders can also interfere with social relationships, as scent and personal memory are tightly interwoven, potentially leading to isolation or depression in affected individuals.
For insight into the broader implications of sensory issues on life and learning, consider reading about The Impact of Sensory Issues on Academic Performance.
Treatment and Management Strategies
There is no one-size-fits-all approach to treating olfactory processing disorders, but there are several strategies that can help individuals manage their symptoms:
- Olfactory Training: Similar to physical therapy for the nose, this involves sniffing various scents regularly to potentially improve the sense of smell.
- Safety Strategies: Using smoke detectors or gas leak detectors can help compensate for the inability to detect hazardous smells.
- Nutritional Guidance: Working with a dietitian can ensure that those with olfactory issues maintain a balanced diet, despite potential changes in taste and flavor perception.
- Supportive Therapies: Counseling or support groups can assist individuals in coping with the emotional and psychological impacts of their condition.
For a deeper dive into the integration of sensory therapies, you might find The Benefits of Sensory Integration in Occupational Therapy particularly enlightening.
Advances in Technology
Recent technological advances have provided new avenues for diagnosing and managing olfactory disorders. Digital olfactometers and scent synthesizers, for instance, offer sophisticated means to test and stimulate the olfactory system. In addition, mobile applications can help track symptoms and treatment progress.
To explore advancements in this field, Advances in Technology for Sensory Health Screening offers a comprehensive look at the latest developments.
The Role of Multidisciplinary Care
Effectively managing olfactory processing disorders often requires a multidisciplinary approach. This can involve otolaryngologists, neurologists, occupational therapists, and psychologists, each playing a pivotal role in the patient’s care. The collaboration among various healthcare providers ensures that all aspects of the disorder are addressed, from the physical to the emotional.
In the realm of olfactory disorders, the intersection of sensory processing and nutrition is particularly noteworthy. A well-rounded approach to treatment often includes diet modifications, as taste and smell are closely intertwined. For an in-depth exploration of this connection, review The Connection Between Sensory Processing and Nutrition.
External Resources for Further Reading
For those seeking niche and specific resources on olfactory processing disorders and sensory health, the following external websites offer high-quality information:
- Monell Chemical Senses Center: A renowned research institute dedicated to understanding the mechanisms and functions of taste and smell.
- Fifth Sense: A charity specifically for people affected by smell and taste disorders, providing support and information.
- National Institute on Deafness and Other Communication Disorders: This organization offers in-depth resources on various smell disorders and the latest research findings.
Conclusion
Olfactory processing disorders present unique challenges that require comprehensive care and management. With the right combination of medical interventions, technological support, and lifestyle adjustments, individuals with these disorders can lead full and rewarding lives. As research continues to shed light on the complexities of the human olfactory system, the potential for improved treatments and outcomes grows.
Understanding the nuances of these conditions is the first step toward empowerment for those affected. By tapping into resources, embracing new strategies, and fostering a supportive community, managing olfactory processing disorders becomes a journey of resilience and adaptation.