The intricate interplay between our gut health and overall well-being is a fascinating topic that has garnered increasing attention in the medical community. The gut, often referred to as the ‘second brain,’ has a profound impact on our body’s homeostasis, including the complex network of hormones and glands known as the endocrine system. This article delves into the vital connections between gut health and endocrine disorders, offering insights and strategies to maintain optimal health.
Understanding the Gut-Endocrine Axis
The gut-endocrine axis refers to the biochemical signaling that takes place between the gastrointestinal tract and the endocrine system. This relationship is crucial for maintaining balance within the body’s metabolic processes. Disturbances in gut health can lead to significant disruptions in hormone production and regulation, leading to various endocrine disorders.
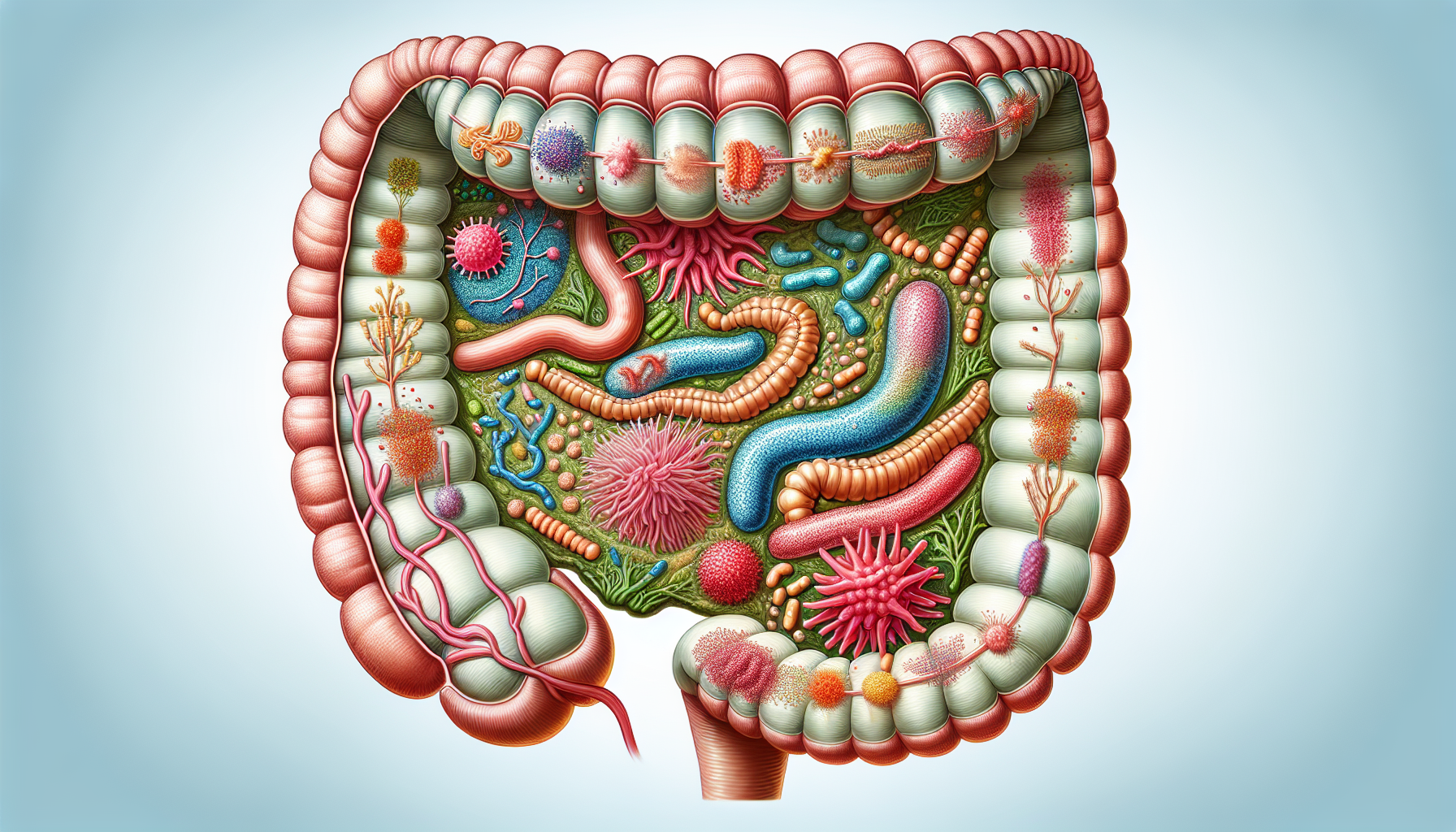
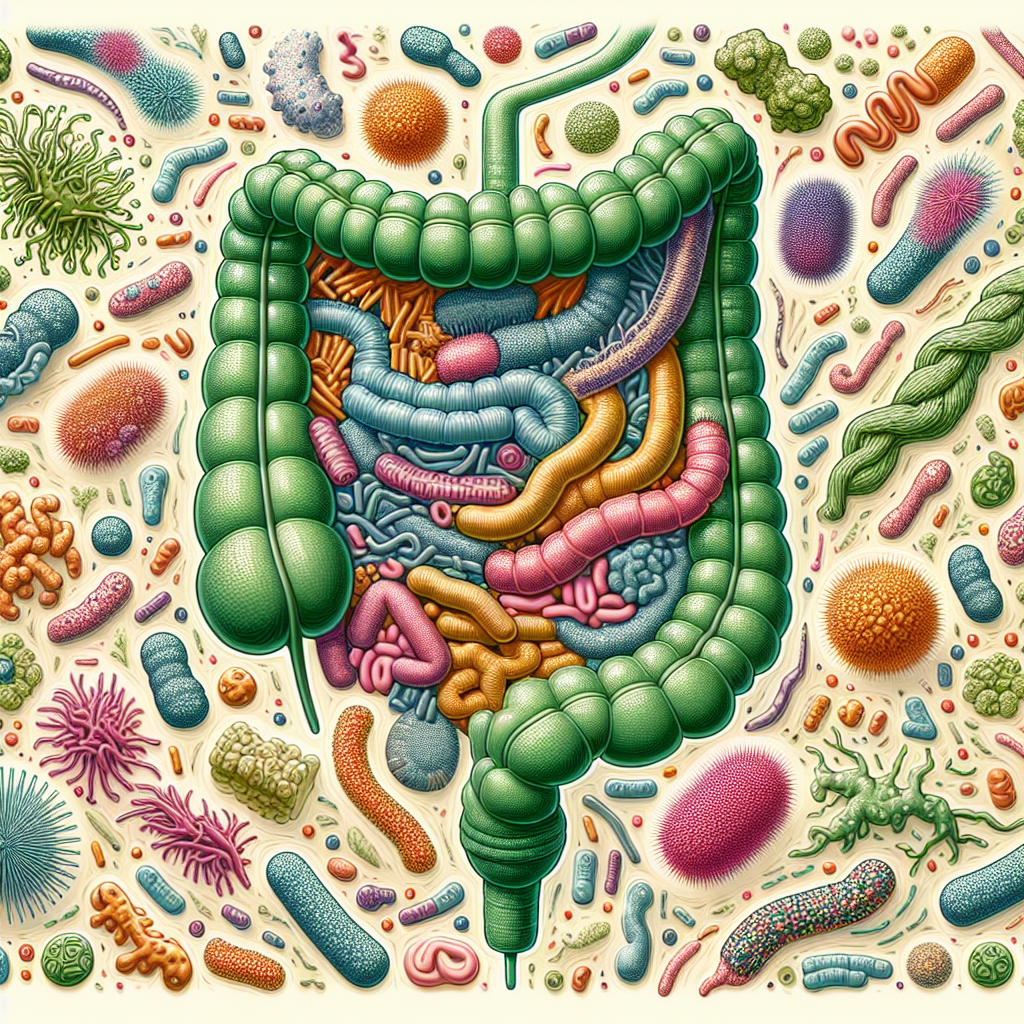
The Role of Gut Microbiota
The human gut is home to trillions of microorganisms, collectively known as the gut microbiota. These microscopic inhabitants are instrumental in many bodily functions, including the metabolism of nutrients, immune system modulation, and the synthesis of certain hormones. For instance, gut bacteria produce short-chain fatty acids (SCFAs) when they ferment dietary fibers. SCFAs have been shown to influence the secretion of gut hormones that regulate appetite and glucose homeostasis.
Gut Dysfunction and Endocrine Disorders
An imbalance in the gut microbiota, known as dysbiosis, can contribute to the pathogenesis of several endocrine disorders, including:
- Diabetes: Dysbiosis may affect insulin sensitivity and glucose metabolism, playing a role in the development of type 2 diabetes.
- Obesity: Altered gut flora can interact with host genes and dietary factors, influencing fat storage and energy balance.
- Thyroid disorders: The gut microbiota can affect the enterohepatic circulation of thyroid hormones, potentially impacting thyroid function.
Dietary Interventions for Gut and Endocrine Health
Diet plays a pivotal role in shaping the composition and function of the gut microbiome, which in turn can have a profound impact on endocrine health. Incorporating specific foods and dietary patterns can help maintain a healthy gut and mitigate the risk of endocrine disorders.
Fiber-Rich Foods
Consuming a diet high in dietary fibers is crucial for nurturing beneficial gut bacteria. These fibers, which are found in fruits, vegetables, and whole grains, can enhance the production of SCFAs, which have been linked to improved insulin sensitivity and energy regulation.
Fermented Foods
Fermented foods like yogurt, kefir, and kimchi introduce beneficial probiotics to the gut. Probiotics can help restore the balance of gut microbiota and have been associated with improved gut barrier integrity and immune function. Learn how to improve gut health with fermented vegetables.
Antioxidant-Rich Foods
Antioxidants found in foods like berries, nuts, and green leafy vegetables can protect the gut lining from oxidative stress and inflammation. Explore the role of antioxidants in gut mucosal health.
Moderate Exercise
Regular, moderate exercise can enhance the diversity of the gut microbiota and is beneficial for both gut and endocrine health. Discover the impact of moderate exercise on digestive function.
Strategies for Restoring Gut Health
Restoring and maintaining gut health is a multifaceted process that often requires lifestyle adjustments and targeted interventions.
Probiotic Supplementation
Probiotic supplements can be an effective way to introduce beneficial bacteria to the gut. These supplements are particularly useful after antibiotic therapy, which can disrupt the natural microbiota balance. Advancements in probiotic supplementation for gut health repair provide further insights into this strategy.
Identifying Food Sensitivities
Food intolerances and sensitivities can contribute to gut inflammation and dysbiosis. Elimination diets or food sensitivity tests can help identify triggers that may be contributing to gut-related endocrine issues. Understanding the gut microbiome’s role in food intolerance offers a deeper understanding of this connection.
Intermittent Fasting
Intermittent fasting has been suggested to benefit the gut microbiota by promoting bacterial diversity and enhancing gut barrier function. This, in turn, may have positive effects on endocrine function, including improved insulin sensitivity. For more information, review the benefits assessed in intermittent fasting for gastrointestinal issues.
External Resources for Further Exploration
To enrich your understanding of the connection between gut health and endocrine disorders, consider exploring these niche resources:
- The Gut Microbiota and Endocrine Disorders, which provides a scientific overview of the topic from the Endocrine Society.
- Gut Microbiota for Health, an initiative by the European Society of Neurogastroenterology & Motility (ESNM) that offers cutting-edge research and education on the gut microbiome.
- The American Gastroenterological Association, which features patient-centered resources on the gut microbiome and its implications for health.
Conclusion
The symbiotic relationship between our gut health and the endocrine system is complex and profound. By fostering a healthy gut microbiota through diet, lifestyle, and targeted interventions, we can potentially prevent and manage endocrine disorders. Continuing research in this field promises to unveil even more connections and therapeutic possibilities, emphasizing the necessity of gut health in our pursuit of holistic well-being.