The human gut microbiome is an intricate and dynamic ecosystem, teeming with trillions of microorganisms that play a fundamental role in our overall health. The complex interplay between these microbes and the host has been the subject of extensive research in recent years, revealing the gut microbiome’s influence on everything from digestion and immunity to mental health and chronic disease risk. However, one aspect of our health that is often overlooked in this microbial conversation is the impact of medications on the gut microbiome, and in turn, how these changes can affect our health outcomes.
The Interconnected Nature of Medications and the Gut Microbiome
Medications are essential in managing health conditions, but they can also have unintended consequences on the gut microbiota. Antibiotics, for example, are well-known for their broad-spectrum activity, which can disrupt the delicate balance of gut bacteria. However, less is known about the effects of other common medications such as non-steroidal anti-inflammatory drugs (NSAIDs), proton pump inhibitors (PPIs), and even oral contraceptives on the microbial composition of the gut.
The gut microbiome plays a crucial role in Digestive Health, and any alterations induced by medications can lead to a range of digestive issues. Dysbiosis, an imbalance in the gut microbiota, is associated with conditions like irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and even obesity. The effects of medication on gut bacteria can also influence the metabolism and effectiveness of drugs, a phenomenon known as the "pharmacomicrobiomics."
Unveiling the Impact of Medications on Microbial Diversity
The diversity of the gut microbiome is a hallmark of good health. A rich and varied microbial community is more resilient and better equipped to perform its many functions. Medications can diminish this diversity, leaving the gut more susceptible to pathogenic colonization and reduced metabolic capacity. For example, the long-term use of PPIs has been linked to decreased microbial richness and an increased risk of Clostridium difficile infections.
To explore this further, let’s delve into the specifics of how certain drug classes interact with our microbial counterparts:
Antibiotics and Microbial Imbalances
Antibiotics are notorious for their capacity to cause significant shifts in the gut microbiota. While they are invaluable in fighting bacterial infections, they often lack specificity, which means they can eradicate beneficial bacteria alongside pathogenic ones. This can lead to a decrease in microbial diversity and give rise to antibiotic-resistant strains of bacteria.
NSAIDs and Gut Microbial Health
NSAIDs, commonly used to manage pain and inflammation, can also affect the gut microbiome. These drugs can cause gastrointestinal side effects and, over time, may lead to changes in the composition of gut bacteria, contributing to the development of conditions such as small intestinal bacterial overgrowth (SIBO) and leaky gut syndrome.
The Influence of Metformin on Gut Microbes
Metformin, a medication used to treat type 2 diabetes, has been shown to modulate the gut microbiome, leading to beneficial changes in some cases. For instance, metformin treatment has been associated with an increase in Akkermansia muciniphila, a bacterium linked to improved metabolic functions.
The Bidirectional Relationship Between the Microbiome and Drug Metabolism
The gut microbiome does not just passively endure the effects of medications; it also actively participates in the metabolism of these substances. Some drugs are directly modified by bacterial enzymes, which can either activate, inactivate, or alter the drug’s efficacy and toxicity. This means that the state of one’s gut microbiome can influence the dosing, effectiveness, and side effects of certain medications.
For instance, the gut bacteria play a significant role in the metabolism of cardiac drugs, thus affecting Cardiovascular Health. The microbial conversion of drugs like digoxin can significantly impact their therapeutic window, necessitating careful monitoring and dosage adjustments.
Strategies to Mitigate the Negative Effects of Medications on the Gut Microbiome
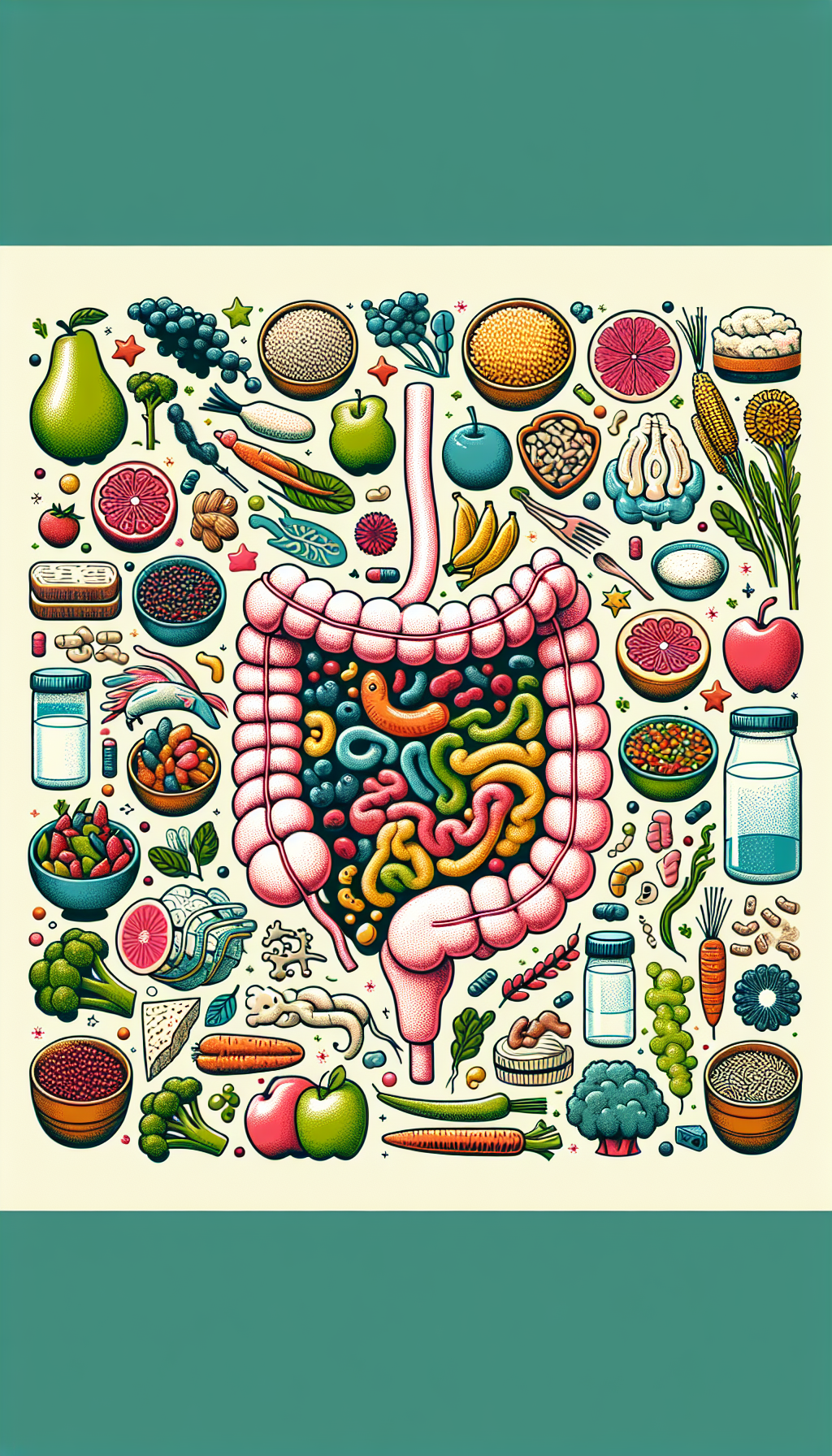
While the use of medications can be essential for managing health conditions, there are strategies that can help mitigate their negative effects on the gut microbiome:
- Probiotics and Prebiotics: These supplements can help restore and maintain a healthy gut microbiota. Probiotics introduce beneficial bacteria, while prebiotics provide the necessary nutrients to support the growth of these microbes.
- Dietary Modifications: A diet rich in fiber, fermented foods, and diverse plant-based foods can promote a robust and resilient microbiome.
- Targeted Drug Development: The advancement of drug formulations that are more selective and less disruptive to the microbiome is an ongoing area of research.
- Personalized Medicine: Tailoring medication choices and dosages based on an individual’s gut microbiota could optimize treatment outcomes and minimize adverse effects.
External Resources for Further Exploration
For readers interested in exploring the detailed interactions between specific medications and the gut microbiome, the following resources offer in-depth information:
- Gut Microbiota for Health provides a comprehensive overview of the latest research and insights on the gut microbiome’s role in health and disease.
- The American Gastroenterological Association offers guidelines and clinical resources related to the impact of medications on gastrointestinal health.
- The Pharmacomicrobiomics Portal is a specialized resource focused on how variations in the human microbiome affect the disposition, action, and toxicity of drugs.
Conclusion
The relationship between medications and the gut microbiome is a complex and bidirectional one, with significant implications for health and disease management. As we continue to uncover the nuances of this interplay, it is clear that a more holistic approach to medication use—one that considers the health of our microbial partners—is needed to optimize therapeutic outcomes and maintain overall well-being.
In the quest to understand the full implications of medications on our health, readers may also find the following articles from Avix Health insightful: "Understanding Generic vs. Brand Name Medications," "Managing Chronic Conditions with Medications and Supplements," and "The Rising Trend of Nootropic Supplements for Cognitive Enhancement." These resources provide a broader context for the importance of personalized and informed approaches to medication and supplement use.
As we navigate our health journeys, let us remember that the tiny, unseen inhabitants of our gut play a monumental role in shaping our health destiny. By fostering a symbiotic relationship with our gut microbiome, we can pave the way for a healthier, more vibrant life.