Chronic inflammation of the gastrointestinal (GI) tract is a persistent condition that can fundamentally disrupt the intricate balance of our digestive system. Understanding how this inflammation impacts the gastrointestinal mucosa is critical not only for individuals suffering from related illnesses but for anyone concerned with maintaining long-term digestive health.
The Role of Gastrointestinal Mucosa in Digestive Health
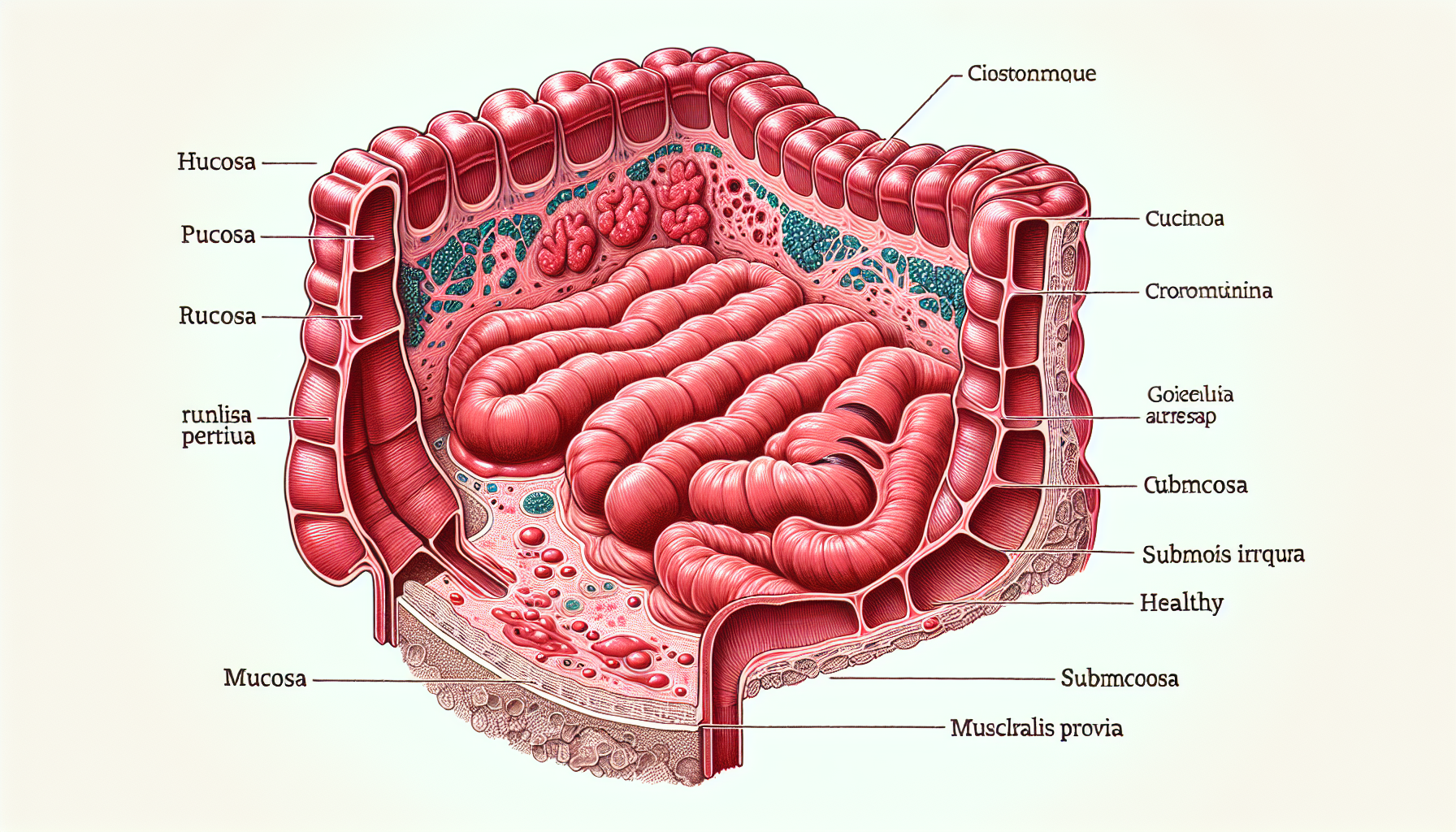
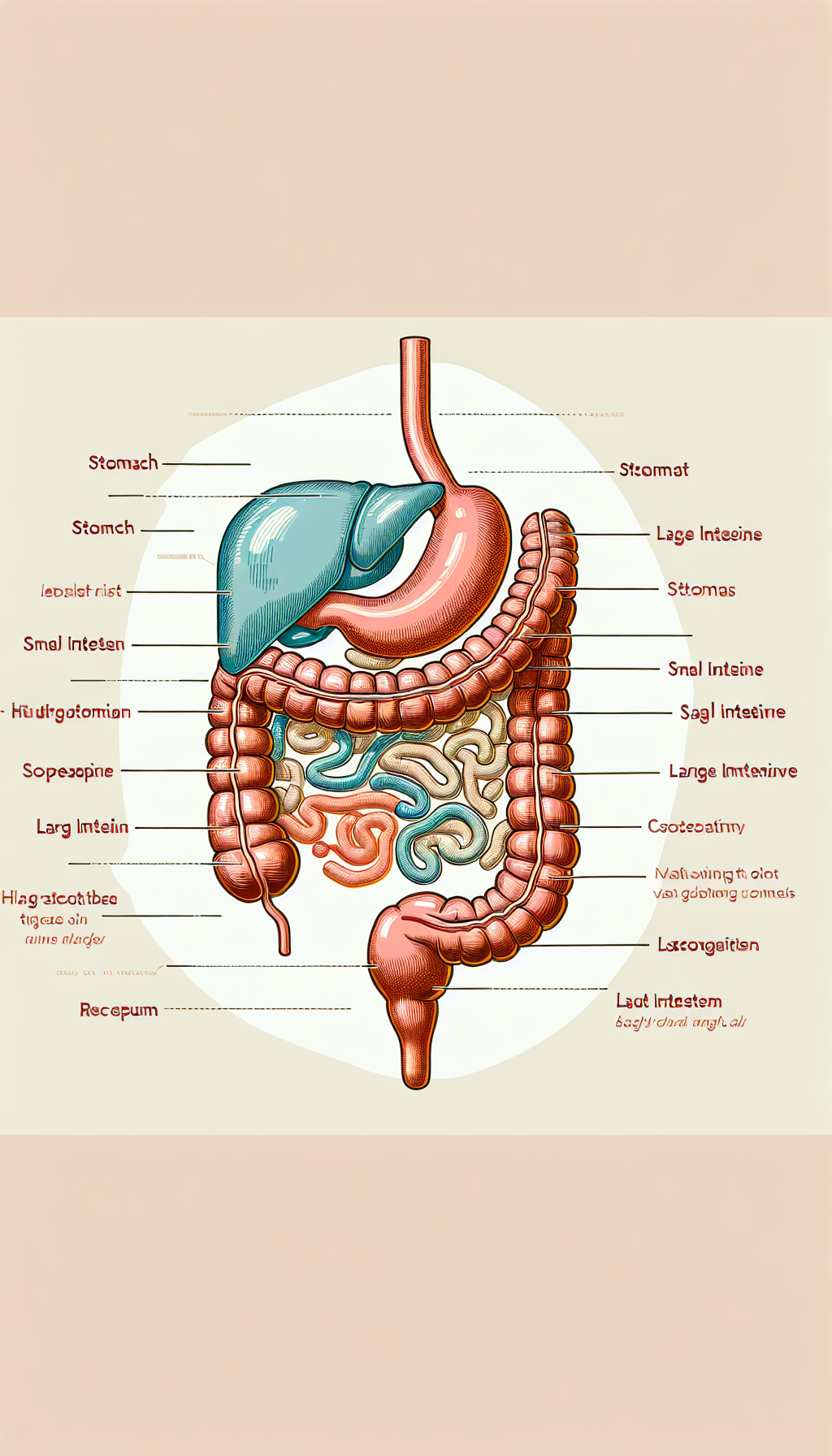
The GI mucosa is a vital barrier and interface between the external environment and the internal milieu of the body. It’s responsible for nutrient absorption and protecting the body from harmful substances. This lining contains specialized cells that secrete mucus, digestive enzymes, and hormones, all of which are essential for proper digestion and overall health.
When the mucosa is healthy, it efficiently performs these tasks, but chronic inflammation can significantly compromise its function. Persistent inflammation can lead to a breakdown in the physical barrier, resulting in increased permeability, often referred to as "leaky gut," which allows pathogens and toxins to enter the bloodstream.
Causes and Consequences of Chronic Inflammation
Chronic inflammation in the GI tract can arise from various sources, including long-term use of certain medications, autoimmune disorders, chronic infections, and lifestyle factors such as diet and stress. Consequences of chronic inflammation include:
- Altered gut microbiota
- Impaired nutrient absorption
- Increased risk of developing food intolerances and allergies
- Propensity towards GI disorders like inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS)
The disruption to the gut microbiota is of particular concern as it plays a pivotal role in immune system modulation and overall health.
Addressing Inflammation Through Diet and Lifestyle
A proactive approach to managing inflammation involves dietary changes and lifestyle modifications. Incorporating anti-inflammatory foods, such as omega-3 fatty acids found in fish and flaxseeds, is a beneficial start. Additionally, the inclusion of dietary fibers can be particularly helpful in maintaining intestinal barrier function, as explained in the article on How Dietary Fibers Affect Intestinal Barrier Function.
Regular physical activity and stress reduction techniques, such as meditation and adequate sleep, also play a crucial role in managing inflammation.
Advancements in Probiotic Supplementation
Probiotics are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host. Advances in probiotic supplementation have shown promise in repairing gut health. Probiotics help restore the balance of good bacteria in the gut, which can be disrupted by chronic inflammation. For more details on this topic, refer to the article on Advancements in Probiotic Supplementation for Gut Health Repair.
The Link Between Gut and Systemic Health
The health of the GI mucosa has far-reaching implications beyond the digestive system. Chronic inflammation of the mucosa can affect systemic health, including skin health, potentially contributing to conditions such as acne, eczema, and psoriasis. This connection is further explored in the article about The Link Between Gut Health and Skin Appearance.
External Resources Supporting Gut Health
To further understand the impact of chronic inflammation on the GI mucosa, it is helpful to consult niche resources that delve into the scientific and clinical aspects of this condition. For example:
- The International Foundation for Gastrointestinal Disorders provides a wealth of information on GI diseases, including those caused by chronic inflammation.
- The Gut Foundation offers resources on maintaining a healthy digestive system and the effects of inflammation.
- Research on the gut-brain axis from reputable academic journals can offer insight into how GI inflammation may affect mental health and cognitive functions.
Innovative Interventions and Treatments
With advancements in medical research, new interventions and treatments targeting chronic inflammation of the GI tract are emerging. These include novel anti-inflammatory drugs, fecal microbiota transplants, and targeted dietary interventions that are tailored to the individual’s gut microbiome.
The medical community is also exploring the benefits of intermittent fasting for gastrointestinal issues, which can play a role in reducing inflammation and improving gut health. More on this can be found in the article about Assessing the Benefits of Intermittent Fasting for Gastrointestinal Issues.
The Future of GI Health Management
Looking ahead, the focus on personalized medicine and precision nutrition holds great promise for managing chronic inflammation in the gastrointestinal mucosa. Understanding an individual’s genetic predisposition, microbiota composition, and lifestyle factors will allow for more targeted and effective interventions.
Conclusion
Chronic inflammation of the GI mucosa is a complex condition with significant implications for overall health. By understanding the causes and consequences, adopting anti-inflammatory lifestyle choices, and leveraging advancements in treatments, individuals can mitigate the effects of this condition and maintain a healthy digestive system. As research continues to evolve, the future of GI health management looks to be increasingly personalized and effective, offering hope to those affected by chronic inflammation.