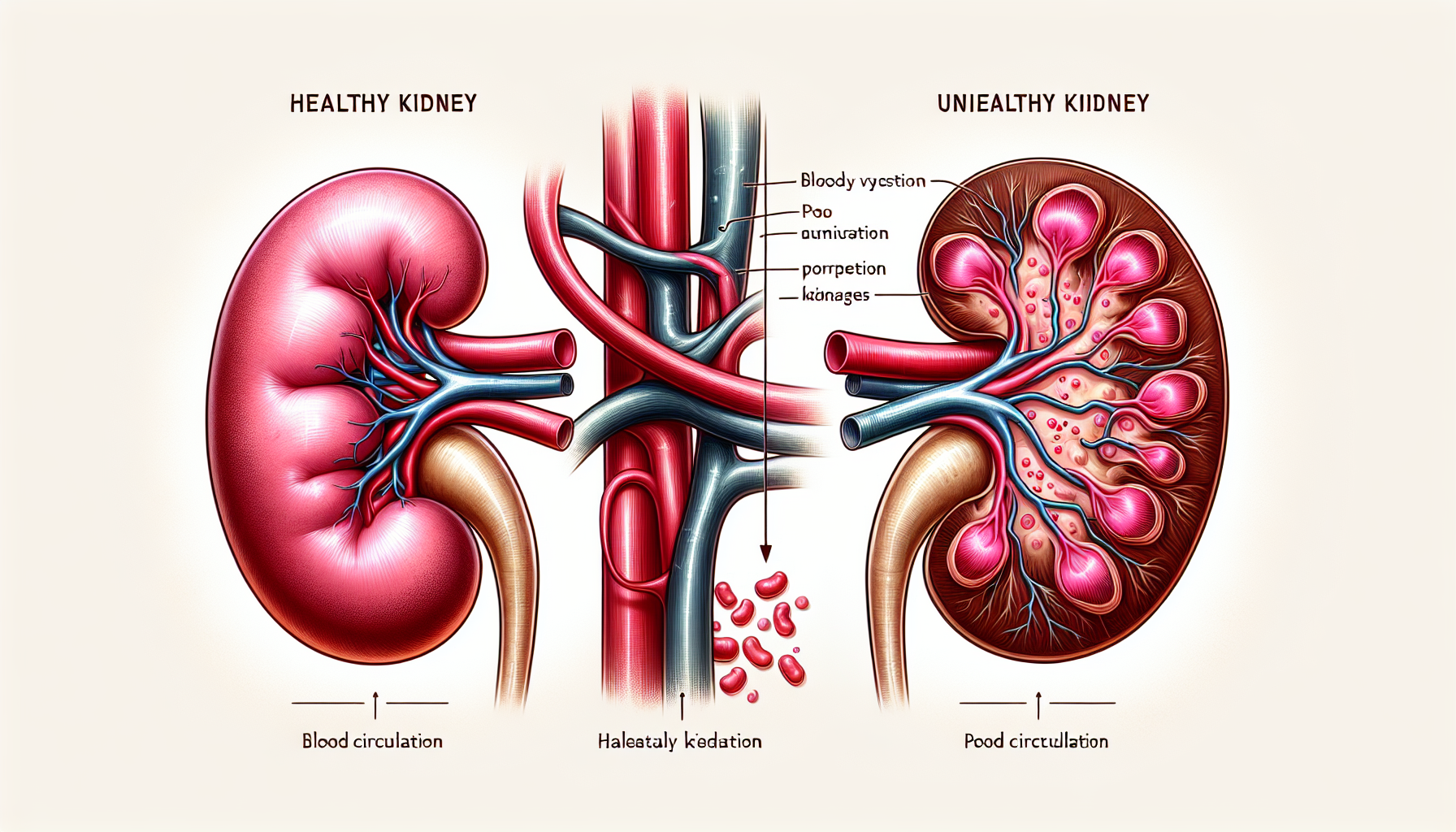
Chronic kidney disease (CKD) is a progressive condition that signifies the gradual loss of kidney function over time. It is a global health concern with a high prevalence, affecting millions of individuals worldwide. As the kidneys fail to perform their essential duties effectively, such as filtering waste and excess fluids from the blood, the repercussions extend far beyond the urinary system. One of the most significant impacts of CKD is on cardiovascular health, creating a complex interplay between heart and kidney functions.
The Kidney-Heart Connection
The kidneys and the heart work in tandem to maintain hemodynamic stability and manage blood pressure, with each influencing the other’s function. Kidney impairment can lead to the accumulation of fluid and waste products, contributing to high blood pressure, a major risk factor for cardiovascular diseases (CVD). Furthermore, CKD can result in changes to the heart’s structure and function, leading to conditions such as left ventricular hypertrophy and heart failure.
The importance of cardiovascular health in the context of CKD cannot be overstated. For comprehensive information on maintaining a healthy heart, Avix Health’s Cardiovascular Health resource provides valuable insights.
Understanding the Impact of CKD on the Heart
CKD affects cardiovascular health through a variety of mechanisms. The following are some of the key ways in which CKD exerts its influence:
Hypertension
With the kidneys’ diminished ability to regulate fluid and sodium balance, blood volume increases, leading to elevated blood pressure. Hypertension exacerbates kidney damage and also increases the strain on the heart, potentially leading to hypertensive heart disease.
Uremic Toxins
As kidney function declines, uremic toxins accumulate in the bloodstream. These toxins can induce inflammation and oxidative stress, both of which are detrimental to cardiovascular tissues, potentially leading to atherosclerosis and other heart diseases.
Anemia
CKD often results in anemia due to reduced erythropoietin production, necessary for red blood cell formation. Anemia decreases oxygen delivery to tissues, forcing the heart to work harder to compensate, which can lead to cardiac complications.
Mineral and Bone Disorders
Disrupted phosphate and calcium regulation can lead to vascular calcification and stiffening of the arteries, increasing the risk of heart disease. This aspect of CKD is closely associated with bone health. For further details on maintaining strong bones, Bone Health provides additional guidelines.
Prevention and Management Strategies
Managing CKD and its cardiovascular implications requires a multifaceted approach:
Blood Pressure Control
Controlling blood pressure is crucial in slowing the progression of CKD and preventing heart complications. Lifestyle modifications and medications, such as ACE inhibitors or angiotensin receptor blockers, are often prescribed.
Management of Uremic Toxins
Dialysis or kidney transplantation may be necessary to manage toxin levels in advanced CKD. A healthy diet and medications can also help control the buildup of these toxins.
Treating Anemia
Erythropoiesis-stimulating agents and iron supplements can be used to treat anemia associated with CKD, thereby reducing the risk of cardiovascular stress.
Addressing Mineral Imbalances
Phosphate binders and vitamin D analogs can help manage mineral and bone disorders, reducing the risk of vascular calcification.
Lifestyle Modifications
Dietary changes, exercise, and smoking cessation are all essential components of managing CKD and its impact on cardiovascular health. For more insights on integrating healthy practices, the article Improving Cardiovascular Health with Mindfulness Practices offers valuable advice.
The Role of Diet in CKD and Cardiovascular Health
Diet plays a pivotal role in managing CKD and its cardiovascular consequences. Limiting intake of sodium, potassium, and phosphorus is recommended to ease the burden on the kidneys and reduce the risk of heart disease. A focus on heart-healthy foods, such as those rich in omega-3 fatty acids, can offer dual benefits. The article on The Importance of Omega-3 Fatty Acids for Heart Health delves deeper into this topic.
Current Research and Innovations
Research continues to unravel the complex relationship between CKD and cardiovascular health. Recent studies have highlighted the potential of novel biomarkers for early detection and the benefits of targeted therapies. Additionally, innovations in wearable technology for monitoring heart health can provide valuable data for individuals with CKD. The significance of these advancements is explored in Innovative Wearable Tech for Heart Rate Monitoring.
External Resources for Further Reading
- The National Kidney Foundation (NKF) offers comprehensive information on CKD and its management.
- The American Heart Association (AHA) provides detailed resources on cardiovascular health and disease prevention.
- The International Society of Nephrology (ISN) is a valuable resource for the latest research and guidelines on kidney health.
Conclusion
CKD poses a significant risk to cardiovascular health, necessitating increased awareness and proactive management. Understanding the interconnectedness of kidney and heart functions is essential for patients and healthcare providers alike. Through effective management strategies, lifestyle changes, and advancements in medical research, individuals with CKD can mitigate the impact on their cardiovascular health and enhance their overall well-being.