Chronic inflammatory conditions are pervasive health issues that affect millions of individuals globally. While commonly linked to their primary symptoms and complications, such as joint pain in arthritis or gastrointestinal distress in Crohn’s disease, the systemic effects of chronic inflammation can extend far beyond the initially affected organ systems. Among these, the cardiovascular system is notably impacted, with inflammation serving as both a marker and a mediator of heart disease.
The Link Between Inflammation and Cardiovascular Health
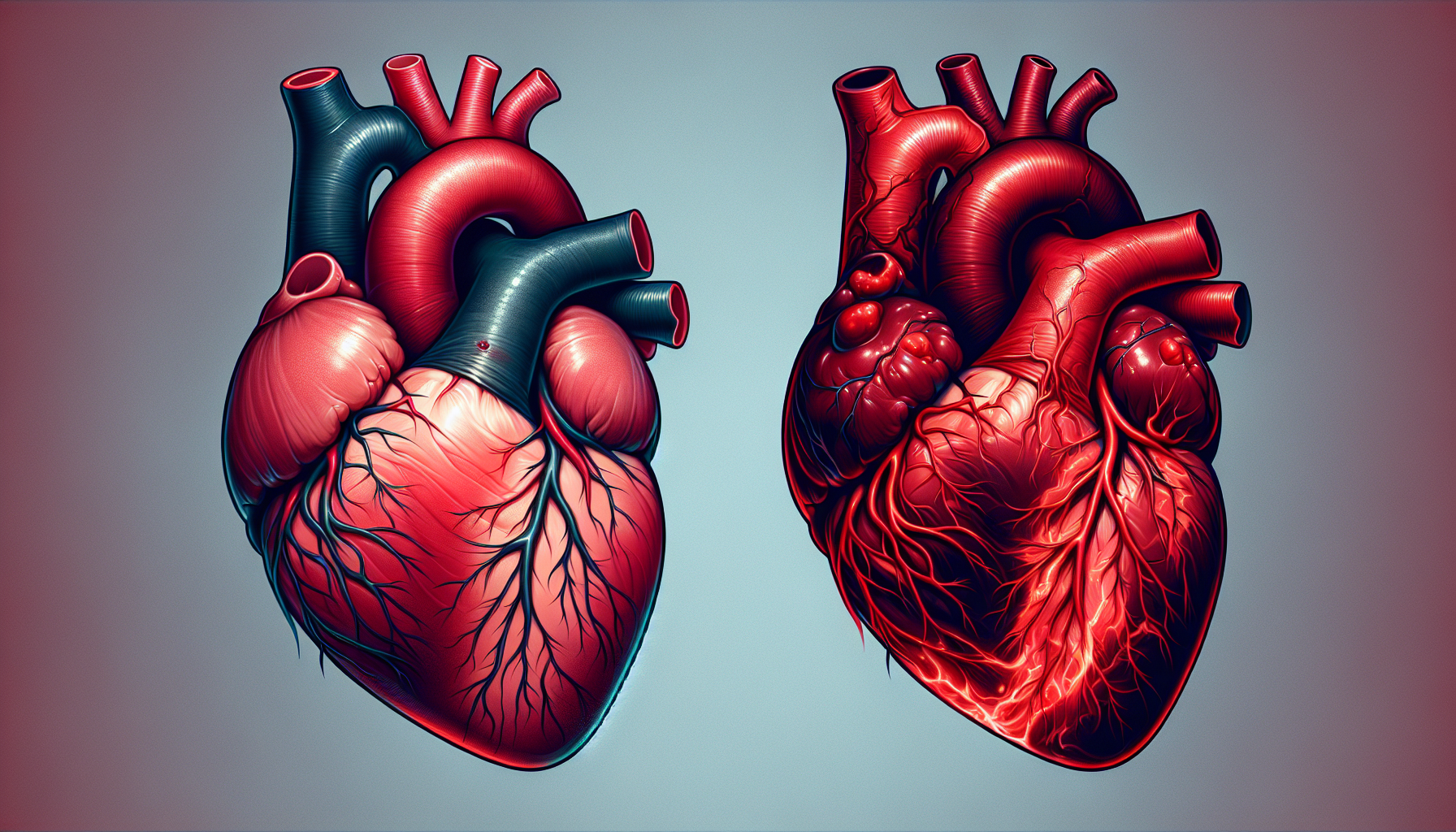
The cardiovascular system, consisting of the heart and blood vessels, is integral to the sustained well-being of every bodily function. It is responsible for the delivery of oxygen and nutrients to tissues and the removal of waste products. Chronic inflammatory conditions disrupt this harmonious system, leading to a cascade of events that can culminate in serious cardiovascular diseases (CVDs).
Inflammation is a natural part of the body’s defense mechanisms, a response triggered to fight infection and promote healing. However, when inflammation becomes chronic, it can cause damage to blood vessels, leading to atherosclerosis—the buildup of plaque in the arteries. This plaque buildup is a significant risk factor for heart attacks, strokes, and other cardiovascular complications.
Understanding the Mechanisms
At the molecular level, chronic inflammation is characterized by the persistent activation of inflammatory pathways and the production of cytokines—proteins that regulate immune and inflammatory responses. These cytokines, including tumor necrosis factor-alpha (TNF-alpha) and interleukins, can have direct and indirect effects on the cardiovascular system.
For example, they can encourage the production of molecules that make the blood more prone to clotting, contribute to the dysfunction of endothelial cells that line the blood vessels, and stimulate the formation of fatty streaks that can evolve into atherosclerotic lesions.
Implications for Patients with Chronic Inflammatory Conditions
Patients with conditions such as rheumatoid arthritis, psoriasis, and systemic lupus erythematosus are at a heightened risk of developing CVDs. This risk is compounded by the fact that these conditions often require treatments with drugs that can have cardiovascular side effects, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids.
For a deeper understanding of how chronic conditions affect overall health, the article on Cardiovascular Health provides extensive insights into maintaining a healthy heart and circulatory system.
Strategies to Mitigate Cardiovascular Risk
Individuals with chronic inflammatory conditions should work closely with their healthcare providers to manage both their primary condition and their cardiovascular risk factors. This includes:
- Regular Monitoring: Regular cardiac screening is essential. For those at high risk, The Benefits of Regular Cardiac Screening for High-Risk Individuals offers valuable information on detecting potential heart issues early on.
- Lifestyle Modifications: Engaging in moderate exercise, following a heart-healthy diet, and avoiding smoking can all help reduce cardiovascular risk. The role of diet is further explored in the article, Tackling Inflammatory Heart Diseases with Anti-inflammatory Diets.
- Medication Management: Utilizing drugs that have dual benefits, such as certain statins that can lower cholesterol and also have anti-inflammatory properties, can be advantageous.
The Role of Diet in Managing Inflammation
Diet plays a critical role in managing chronic inflammation. Anti-inflammatory diets, rich in fruits, vegetables, whole grains, lean protein, and healthy fats, such as omega-3 fatty acids, can help reduce inflammation levels. Conversely, diets high in refined sugars, trans fats, and processed foods can exacerbate inflammatory processes.
Exercise as a Potent Anti-inflammatory
Regular physical activity is another powerful tool against chronic inflammation. Exercise can help improve endothelial function, lower blood pressure, and reduce cytokine production. For those new to exercise, Engaging in Cardiovascular Fitness: A Guide for Beginners is an excellent resource to get started.
External Resources for Further Information
In addition to the resources provided by Avix Health, there are numerous external sources that offer in-depth knowledge on the connection between chronic inflammation and cardiovascular health:
- The American Heart Association provides extensive educational materials on how systemic inflammation affects heart health.
- The National Heart, Lung, and Blood Institute offers research and guidelines on the management of heart diseases, including those influenced by inflammation.
- The Arthritis Foundation has specialized resources discussing the cardiovascular risks associated with autoimmune and inflammatory forms of arthritis.
- Scholarly articles from peer-reviewed journals, accessible through databases like PubMed, delve into the latest research findings on the subject matter.
Conclusion
Understanding the cardiovascular implications of chronic inflammatory conditions is crucial for both patients and healthcare providers. By recognizing the interplay between inflammation and heart health, implementing preventative strategies, and utilizing resources available, individuals can significantly reduce their risk of cardiovascular complications. Maintaining a holistic approach that encompasses diet, exercise, and appropriate medical interventions is the key to managing the systemic effects of chronic inflammation on the heart.