Menopause is a significant milestone in a woman’s life often accompanied by various physiological changes that can impact overall health. One of the most critical areas affected is bone health. The decline in estrogen levels during menopause can lead to a decrease in bone density, increasing the risk of osteoporosis and fractures. This comprehensive guide explores the risks associated with bone health in menopausal women and offers actionable solutions to maintain and improve skeletal strength.
Understanding Bone Density and Menopause
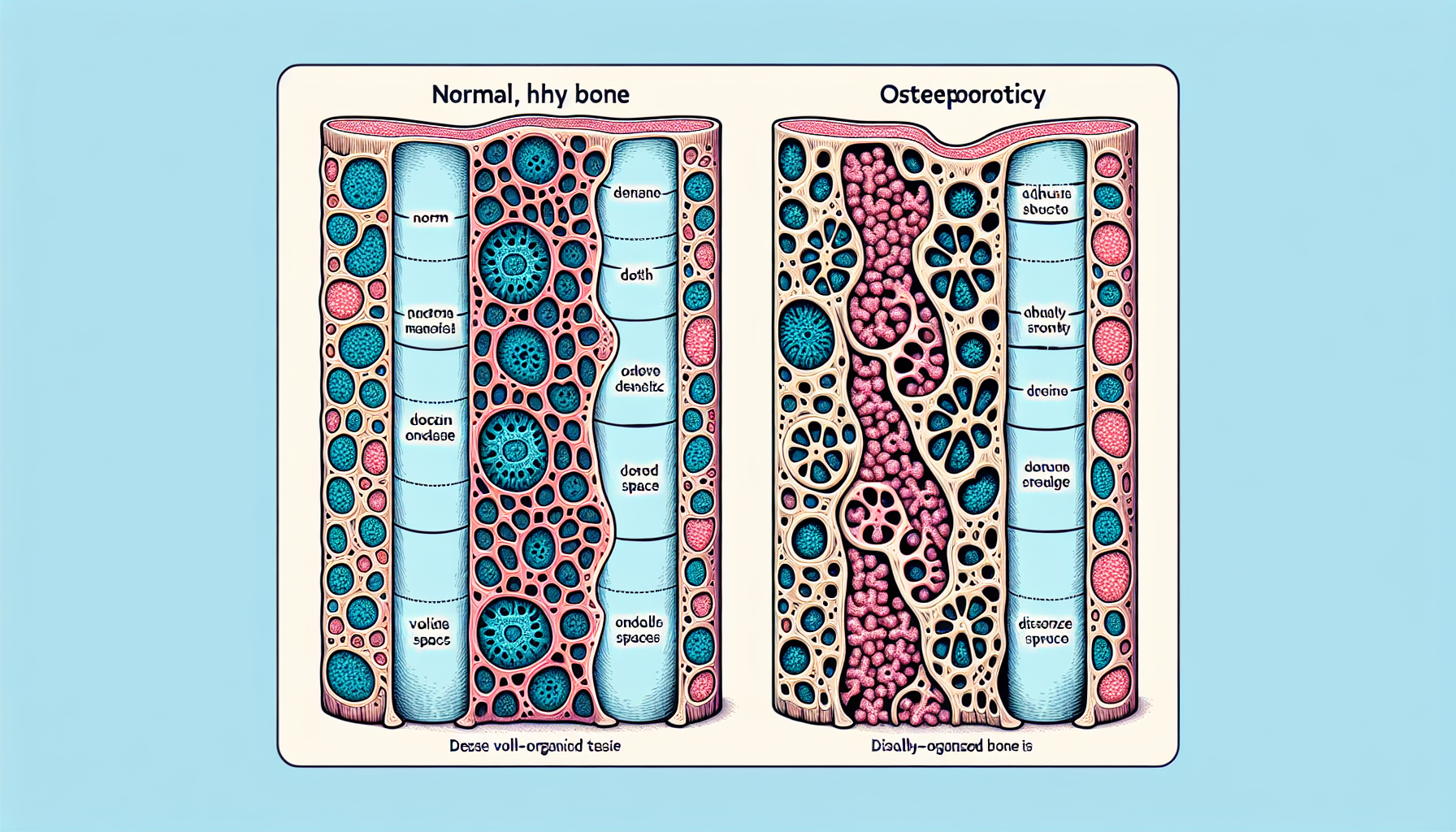
Bone density refers to the amount of bone mineral in bone tissue, and it is a primary indicator of bone strength and health. During menopause, the decrease in estrogen production significantly affects the body’s ability to absorb and retain calcium, a crucial mineral for bone formation and maintenance. Without sufficient estrogen, bones lose density more quickly, becoming porous, brittle, and prone to fracture.
For a deeper understanding of bone health and its importance, readers can explore Bone Health, which provides extensive information on how to maintain strong and healthy bones throughout different stages of life.
Identifying the Risks
Menopausal women face an increased risk of developing osteoporosis, a condition characterized by weakened bones. Recognizing the early signs and risk factors is vital for prevention and management. These include:
- A family history of osteoporosis
- Early menopause (before age 45)
- A history of bone fractures
- A small, thin frame
- Smoking and excessive alcohol consumption
- Certain medications and medical conditions
It is crucial to evaluate personal risk factors and seek professional guidance for appropriate bone density scans, as discussed in Evaluating the Effectiveness of Different Bone Density Scans.
Nutritional Interventions
Diet plays a pivotal role in bone health. Key nutrients include calcium, vitamin D, magnesium, and phosphorus. Women who are lactose intolerant often struggle to meet their calcium needs, but there are alternative strategies to ensure adequate intake, which can be found in Bone Health Strategies for Those with Lactose Intolerance.
For those seeking to enhance their diet, it’s essential to consider the role of omega-3 fatty acids. These nutrients are known for their anti-inflammatory properties and have been linked to improved bone density. The intricate relationship between these fatty acids and bone health can be explored further in The Role of Omega-3 Fatty Acids in Bone Density.
Lifestyle Modifications
Physical activity, particularly weight-bearing exercises like walking, jogging, and strength training, can help maintain bone density. Engaging in regular exercise not only strengthens the bones but also improves muscle strength, balance, and coordination, reducing the risk of falls and fractures.
Additionally, it’s important to address lifestyle factors such as smoking cessation and moderating alcohol intake, both of which can negatively impact bone density.
Medical Interventions
Hormone Replacement Therapy (HRT) is one option for slowing bone density loss in menopausal women. However, HRT is not suitable for everyone and comes with its own set of risks and benefits. Therefore, it is vital to discuss this option with a healthcare provider to determine the best course of action.
There are also non-hormonal medications available that can help prevent bone loss and reduce the risk of fractures. Bisphosphonates, for example, are commonly prescribed to prevent and treat osteoporosis.
Supplements and Alternative Therapies
Calcium and vitamin D supplements can be beneficial for those who find it challenging to get enough from their diet. Other supplements that may support bone health include vitamin K2, which plays a role in bone metabolism. The significance of vitamin K2 and its impact on bone health is detailed in The Role of Vitamin K2 in Bone Metabolism.
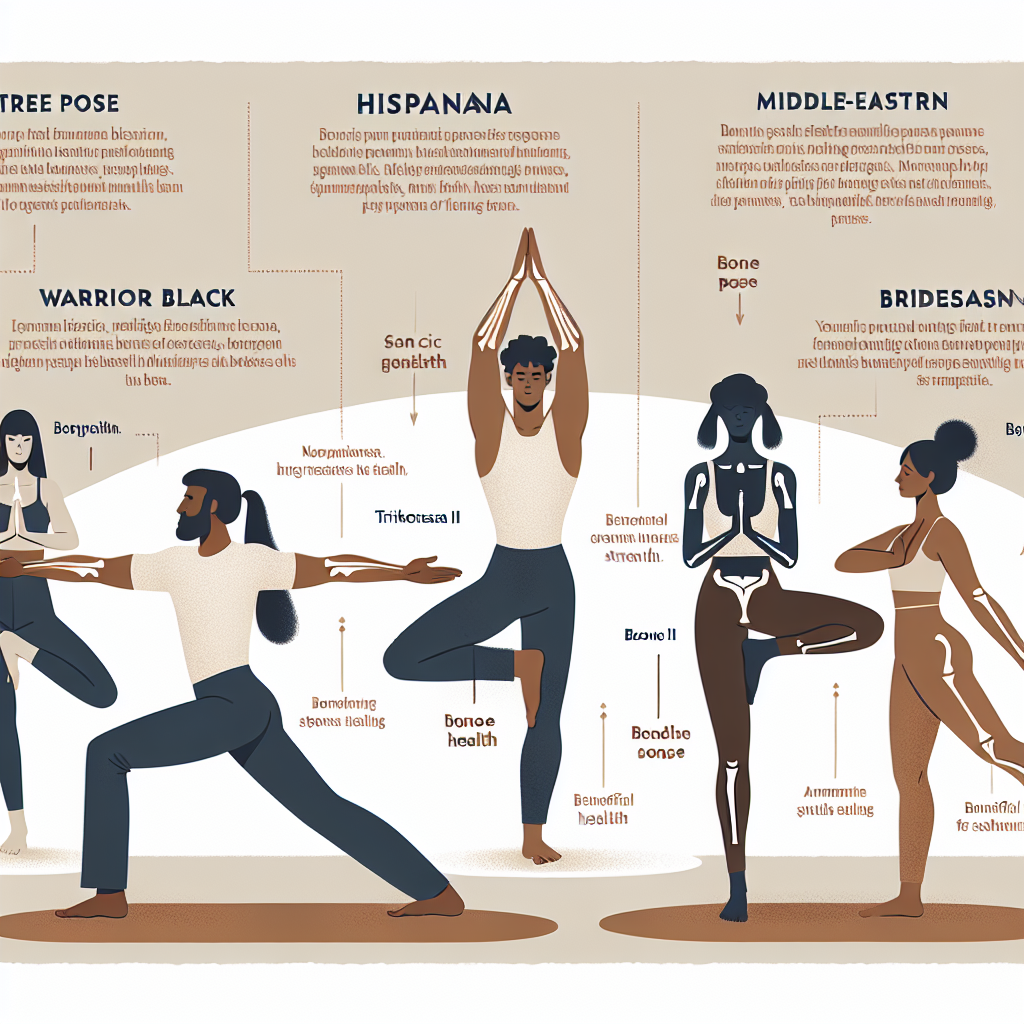
Alternative therapies like yoga have also been shown to be beneficial for bone health. Yoga can improve flexibility, balance, and strength, with some studies suggesting that it may also help increase bone density. For an evaluation of the benefits of yoga for bone health, visit Evaluating the Benefits of Yoga for Bone Health.
Seeking Professional Guidance
Regular check-ups with a healthcare provider are crucial for monitoring bone health. Healthcare professionals can provide personalized advice, prescribe medications if necessary, and recommend bone density tests to track bone health over time.
External Resources for Further Reading
For those interested in further exploring the topic, here are several niche and specific external resources that can provide additional insights:
- The North American Menopause Society offers in-depth information on how menopause affects bone health and practical tips for prevention and treatment.
- The International Osteoporosis Foundation provides an online risk assessment tool to help women evaluate their risk for osteoporosis.
- The National Osteoporosis Foundation has comprehensive details on bone density testing and how it can help in the management of bone health.
- The American Bone Health Organization provides a detailed guide on calcium-rich foods that are essential for maintaining strong bones.
In conclusion, menopause is a critical time for focusing on bone health. With informed dietary choices, regular physical activity, appropriate medical interventions, and vigilant monitoring, menopausal women can significantly reduce their risk of osteoporosis and maintain a robust skeletal framework. By taking proactive steps and utilizing the wealth of available resources, a strong foundation for bone health can be established during menopause and beyond.