In the intricate framework of the human body, bones are the bedrock that provide structure, protect organs, anchor muscles, and store calcium. Essential for our mobility and vitality, bone health is a critical aspect of overall wellness that often goes unnoticed until something goes wrong. The importance of maintaining robust bones cannot be overstated, as they are the support system of our bodies, and their well-being has a direct impact on our quality of life. This article aims to explore the complexities of bone health, unraveling the strategies, behaviors, and nutritional guidelines that can fortify our skeletal system throughout the different stages of life.
Understanding Bone Structure and Function
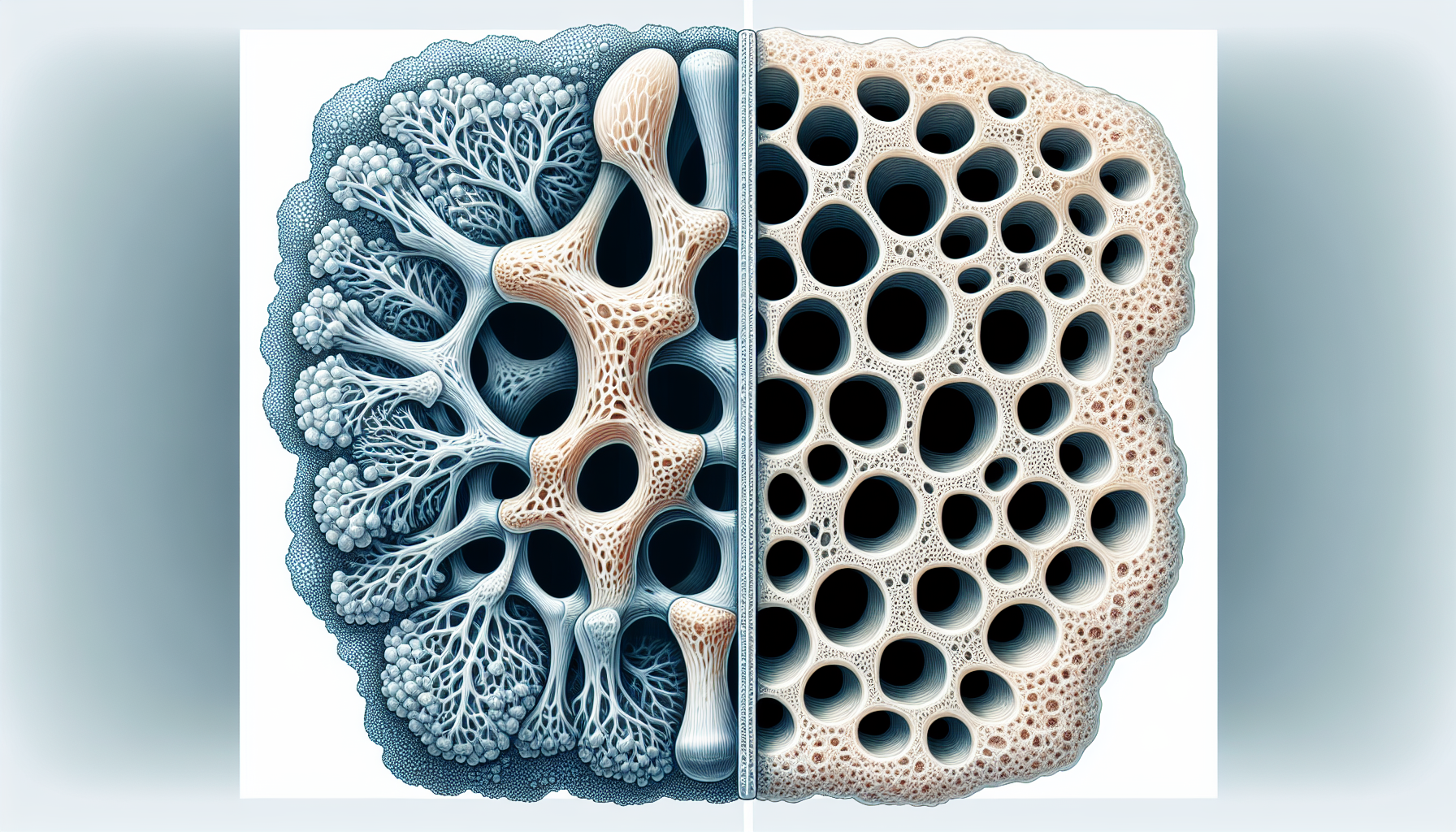
Bones are living, dynamic tissues that undergo continuous turnover through a process called remodeling. This involves the resorption of old bone and the formation of new bone, a balance that is crucial for maintaining bone strength and density. The human skeleton is composed of two types of bone tissues:
- Cortical bone, which is dense and forms the outer shell of bones, providing most of the structural support.
- Trabecular bone, which is spongy and found at the ends of long bones, within the spinal vertebrae, and inside flat bones like the pelvis. It is more susceptible to changes over time and plays a significant role in bone metabolism.
The Life Cycle of Bone
Bone health is not static; it changes throughout a person’s life. The following stages are key to understanding how bone density and strength evolve:
- Growth: Childhood and adolescence are periods of rapid bone growth, with most individuals reaching their peak bone mass by their late twenties.
- Maintenance: From peak bone mass until around age 50, the goal is to maintain bone density and strength through a balanced diet and regular exercise.
- Decline: As we age, bone resorption begins to outpace bone formation, leading to a gradual loss in bone mass and density.
Factors Affecting Bone Health
Several factors can influence bone health, many of which are within our control. These include:
- Calcium Intake: Adequate calcium is critical for building and maintaining strong bones.
- Vitamin D Levels: Vitamin D is essential for calcium absorption in the bones.
- Physical Activity: Regular weight-bearing exercise stimulates bone formation and strengthens existing bone tissue.
- Hormonal Balance: Hormones, particularly estrogen in women, play a significant role in bone density.
- Lifestyle Choices: Smoking and excessive alcohol consumption can accelerate bone loss.
- Medications: Certain medications can have adverse effects on bone density.
Recognizing the interplay of these factors is the first step in developing a proactive approach to bone health.
Calcium: The Cornerstone of Bone Health
Calcium is the most abundant mineral in the body and is vital for several physiological processes. For bone health, it serves as the primary building block. Adults typically require between 1,000 to 1,200 milligrams of calcium per day, with higher amounts recommended for teens, postmenopausal women, and the elderly. Dietary sources of calcium include:
- Dairy products such as milk, cheese, and yogurt
- Leafy green vegetables like kale and broccoli
- Fortified foods such as cereals, orange juice, and plant-based milks
- Fish with edible soft bones, such as sardines and canned salmon
When dietary intake is insufficient, calcium supplements can be considered; however, it is always best to consult with a healthcare provider before starting any supplementation.
The Role of Vitamin D
Vitamin D is essential for calcium absorption; without it, our bodies cannot effectively utilize the calcium we consume. Sun exposure is a natural source of vitamin D, as the skin synthesizes it when exposed to sunlight. However, many factors such as geographic location, skin pigmentation, and lifestyle can limit sun exposure, leading to vitamin D deficiency. Food sources of vitamin D include:
- Fatty fish like salmon, mackerel, and tuna
- Egg yolks
- Fortified foods and beverages
Supplementation can be necessary for those with limited sun exposure or dietary intake. The recommended daily allowance (RDA) for vitamin D varies depending on age, sex, and life stage, with general guidelines suggesting 600 to 800 IU per day for most adults.
Weight-Bearing Exercise: A Pillar of Strength
Physical activity, specifically weight-bearing exercise, is a linchpin in maintaining and improving bone health. These activities force the body to work against gravity, stimulating bone formation and strengthening muscles that support the bones. Examples of weight-bearing exercises include:
- Walking, hiking, and jogging
- Tennis and basketball
- Dancing and aerobics
- Resistance training such as weightlifting
Incorporating a mix of these activities into a regular exercise routine can have profound benefits for bone density, especially when started at a young age and continued throughout life.
Hormones and Bone Density
The hormonal milieu within our bodies has a profound impact on bone health. Estrogen, in particular, is known for its bone-protective effects. In women, the decline in estrogen levels during menopause can lead to a rapid decrease in bone density, increasing the risk of osteoporosis. Men also experience a gradual decline in sex hormones with age, which can affect their bone health, albeit typically to a lesser extent.
Other hormones that influence bone health include:
- Testosterone: In both men and women, this hormone helps maintain bone thickness.
- Parathyroid hormone: Regulates calcium levels within the blood and bone turnover.
- Cortisol: High levels of this stress hormone can lead to bone loss.
Understanding these hormonal influences can guide strategies for maintaining bone health as we age.
Lifestyle Choices Impacting Bones
Choices we make in our daily lives can either support or undermine our bone health. Smoking, for instance, interferes with the balance of bone remodeling by reducing blood flow to the bones, slowing the production of bone-forming cells, and impairing the absorption of calcium. Similarly, excessive alcohol consumption can lead to bone loss and increased risk of fractures by inhibiting the production of bone cells and affecting the body’s calcium balance.
It’s also important to consider the impact of certain medications on bone density. Long-term use of corticosteroids, certain anticonvulsants, and some cancer treatments can have detrimental effects on bone health. If you are taking any of these medications, it is crucial to discuss bone health with your healthcare provider and take steps to mitigate these effects.
To promote bone health through lifestyle choices:
- Avoid smoking and limit alcohol consumption.
- Maintain a healthy weight to reduce the burden on your bones.
- Ensure a balanced diet with adequate calcium and vitamin D.
As we continue to delve into the complexities of bone health, it becomes clear that a multifaceted approach is necessary to maintain strong bones. From understanding the integral role of nutrition and exercise to recognizing the impact of hormones and lifestyle choices, each aspect plays a significant role in cultivating a framework for lifelong bone health. In the following sections, we will explore how genetics, medical conditions, and proactive strategies further influence and support our skeletal system.
Genetic Factors in Bone Health
While lifestyle choices play a significant role in bone health, genetics also have a considerable impact. Studies show that genetic factors can account for up to 80% of the variance in peak bone mass. Certain genes are involved in bone growth and repair, and variations in these genes can affect bone density and susceptibility to osteoporosis.
Major Genes Influencing Bone Density
Several genes are known to influence bone density, including but not limited to:
- COL1A1: This gene encodes type I collagen, the major protein of bone.
- VDR: The Vitamin D receptor gene affects calcium absorption and bone growth.
- ESR1: The estrogen receptor gene plays a role in the regulation of bone density.
- LRP5: Mutations in this gene can lead to conditions with high bone mass or osteoporosis.
Identifying individuals with genetic predispositions to poor bone health can lead to early interventions and personalized treatment plans. Genetic testing for these markers is becoming more common, allowing for more targeted approaches to bone health management.
Medical Conditions Affecting Bone Health
Certain medical conditions can have a profound impact on bone health. These conditions can lead to an increased risk of osteoporosis and fractures. They include:
- Endocrine disorders: Conditions such as hyperthyroidism, hyperparathyroidism, and Cushing’s syndrome can cause bone loss.
- Inflammatory diseases: Rheumatoid arthritis and other chronic inflammatory conditions can lead to reduced bone density.
- Gastrointestinal diseases: Disorders that impair nutrient absorption, such as celiac disease and inflammatory bowel disease, can lead to deficiencies in calcium and vitamin D, affecting bone health.
- Cancer: Certain cancers and treatments, like chemotherapy, can weaken bones.
Management of these conditions often requires a collaborative approach involving various healthcare providers to ensure that bone health is addressed along with the primary illness.
Assessing Bone Health: Diagnostic Tools
To evaluate bone health and diagnose conditions like osteoporosis, healthcare providers use several diagnostic tools:
- Bone Mineral Density (BMD) Tests: A dual-energy x-ray absorptiometry (DEXA) scan is the most common test for measuring BMD.
- FRAX Score: The FRAX tool uses information about bone density and other risk factors to predict the 10-year risk of fracture.
- Bone Markers: Blood and urine tests can measure biochemical markers of bone turnover.
These assessments help in determining the need for treatment and in monitoring the effectiveness of interventions over time.
Proactive Strategies for Bone Health
Proactive measures are essential in maintaining bone density and reducing the risk of fractures. These strategies include:
- Nutritional Support: Ensuring an intake of bone-supporting nutrients such as calcium, vitamin D, magnesium, and phosphorus.
- Lifestyle Modifications: Adopting habits that support bone health, such as engaging in regular physical activity and avoiding smoking and excessive alcohol consumption.
- Fall Prevention: Implementing safety measures to prevent falls, especially in older adults, can significantly reduce the risk of fractures.
Nutritional Guidelines and Supplementation
A balanced diet rich in bone-healthy nutrients is the foundation of good bone health. Here are some dietary guidelines:
- Calcium: Aim for the recommended daily intake through diet, and consider supplements if needed.
- Vitamin D: Seek to get an adequate amount of vitamin D from sunlight exposure, diet, and supplements as necessary.
- Protein: Adequate protein intake is crucial as it is a major component of bone.
- Magnesium and Phosphorus: These minerals are also important for bone health and are found in nuts, seeds, and whole grains.
For those who have difficulty meeting their nutritional needs through diet alone, supplements may be necessary. It is important to discuss supplementation with a healthcare provider to ensure proper dosing and avoid potential interactions with other medications.
Incorporating Weight-Bearing Exercises
Including a variety of weight-bearing exercises in one’s routine can help improve bone health. Here’s a list of effective activities:
- High-impact exercises: Running, jumping rope, and playing high-impact sports can help build and maintain bone density.
- Low-impact exercises: For those who cannot perform high-impact exercises, activities like walking, elliptical training, and low-impact aerobics are beneficial.
- Strength training: Using free weights, resistance bands, or weight machines can help improve muscle mass and bone strength.
- Balance and flexibility exercises: Yoga and tai chi can improve balance and coordination, reducing the risk of falls.
It is advisable for individuals to consult with a healthcare provider before starting a new exercise program, especially if they have health conditions that may affect their ability to exercise safely.
Monitoring and Medication
For those at high risk of osteoporosis or with a diagnosis, monitoring bone density and taking prescribed medications can be critical.
Medications for Bone Health
Several types of medications are used to treat osteoporosis and other bone-related conditions:
- Bisphosphonates: These drugs slow down bone loss and are often the first choice of treatment.
- Denosumab: This medication is a monoclonal antibody that helps to prevent bone resorption.
- Selective Estrogen Receptor Modulators (SERMs): These drugs mimic estrogen’s bone-protective effects in postmenopausal women.
- Parathyroid Hormone Analogues: These drugs stimulate bone formation and are used in people with severe osteoporosis.
Each medication comes with its benefits and risks, so it is essential for patients to discuss these with their healthcare provider to determine the best course of action for their specific situation.
The Role of Hormone Replacement Therapy (HRT)
Hormone replacement therapy can be a powerful tool in the management of menopause-related bone loss in women. Estrogen, sometimes in combination with progesterone, can significantly reduce the risk of osteoporosis and fractures. However, HRT is not suitable for everyone and requires careful consideration of the potential risks, such as the increased risk of certain types of cancer and cardiovascular events.
Regular Monitoring
Individuals with osteoporosis or other conditions that affect bone density should have regular check-ups, including bone density tests, to monitor their bone health. This allows for timely adjustments to treatment plans.
Environmental and Occupational Influences
Environmental and occupational factors can also influence bone health. Exposure to certain chemicals or heavy metals, physically demanding work, or a sedentary lifestyle can all have an impact on bone density.
Addressing Environmental Risks
Awareness of environmental risks includes:
- Reducing exposure to lead and other heavy metals: These can have a negative effect on bone health.
- Limiting exposure to endocrine-disrupting chemicals: Such as bisphenol A (BPA), which can interfere with bone metabolism.
Occupational Health
For those in physically demanding jobs, it is important to:
- Use proper lifting techniques: To avoid injury and ensure bone and joint health.
- Take regular breaks: To prevent repetitive strain injuries which can affect bone and joint health.
Conversely, for those in sedentary occupations, it is crucial to: - Incorporate movement throughout the day: To stimulate bone formation and prevent bone loss.
- Use ergonomic furniture: To support posture and reduce strain on the skeletal system.
As we progress through the intricacies of bone health, it is evident that a comprehensive approach encompassing genetics, medical management, lifestyle, and environmental factors is key to maintaining a robust skeletal system. By understanding the multifaceted nature of bone health, individuals can take proactive steps to ensure their bones remain strong and supportive throughout their lives. By fostering a deeper comprehension of the factors that influence our skeletal framework, we empower ourselves to take charge of our bone health and enhance our overall well-being.
The Importance of Early Intervention
Early intervention in bone health is crucial, as the density and quality of bone mass attained in the early years lay the groundwork for skeletal health throughout life. The focus on bone health should begin in childhood, with an emphasis on proper nutrition and physical activity to maximize peak bone mass. This can have a profound impact on minimizing the risk of osteoporosis and other bone-related issues later in life.
Pediatric Bone Health
Pediatrics is a critical window for bone development, and the following strategies can support this process:
- Nutrition: Ensuring children receive adequate amounts of calcium and vitamin D.
- Physical Activity: Encouraging children to engage in outdoor play and sports to promote bone growth and density.
- Screening: Monitoring growth patterns and bone health in children with a family history of osteoporosis.
The Role of Diet in Bone Health
Diet plays a significant role in maintaining bone health throughout the various stages of life. A diet rich in key nutrients not only supports the structural integrity of bones but also assists in the prevention of bone diseases.
Essential Nutrients for Bone Health
Here are some of the key nutrients necessary for maintaining healthy bones:
- Calcium: A critical component for bone structure and hardness.
- Vitamin D: Facilitates calcium absorption and bone growth.
- Protein: Provides a framework for bone mineralization.
- Magnesium: Works with calcium to form strong bone structure.
- Vitamin K: Vital for bone metabolism and regulating calcium levels.
Dietary Sources of Bone-Building Nutrients
To support the dietary needs for bone health, the following foods should be included in one’s diet:
- Calcium: Dairy products, fortified plant-based milks, leafy greens, and tofu.
- Vitamin D: Fatty fish, fortified foods, and egg yolks.
- Protein: Lean meats, fish, dairy products, and legumes.
- Magnesium: Nuts, seeds, whole grains, and dark chocolate.
- Vitamin K: Green leafy vegetables, such as spinach, kale, and collard greens.
Supplements and Bone Health
While a balanced diet is the best way to obtain essential nutrients, supplements can play a role in bone health, especially when dietary intake is insufficient or in individuals with higher needs.
When to Consider Supplements
Supplements may be considered in the following scenarios:
- Insufficient Dietary Intake: When people are unable to consume enough nutrients through diet alone.
- Increased Requirements: During certain life stages such as adolescence, pregnancy, or old age.
- Medical Conditions: In individuals with diseases that affect nutrient absorption or bone metabolism.
It is important to remember that supplements should not replace a healthy diet and lifestyle. Rather, they should complement them. Additionally, the decision to take supplements should be made under the guidance of a healthcare provider.
Bone Health in Different Life Stages
Bone health concerns vary across different life stages, necessitating tailored approaches for each age group.
Adolescence
During adolescence, the focus should be on maximizing bone mass through:
- Optimal Nutrition: High intake of calcium and vitamin D.
- Physical Activity: Participation in sports and exercise to stimulate bone growth.
Adulthood
In adulthood, maintaining bone density becomes the primary goal through:
- Balanced Diet: Continued emphasis on nutrients important for bone health.
- Regular Exercise: Incorporating both weight-bearing and muscle-strengthening activities.
Senior Years
As individuals enter their senior years, the emphasis shifts to preventing bone loss and fractures by:
- Nutrient-Rich Diet: Especially increased calcium and vitamin D to counteract the natural decline in bone density.
- Fall Prevention: Implementing measures to reduce the risk of falls, such as balance training.
Addressing Gender-Specific Issues in Bone Health
Gender-specific factors, such as hormonal changes in women during menopause or the gradual decrease in testosterone in men, can significantly impact bone health. The following are considerations for addressing these issues:
Women’s Bone Health
For women, particularly those who are postmenopausal, the following strategies are important:
- Calcium and Vitamin D: Ensuring adequate intake to counteract increased bone resorption after menopause.
- HRT Consideration: Discussing the potential benefits and risks of hormone replacement therapy with a healthcare provider.
Men’s Bone Health
Men, while generally experiencing less dramatic bone loss with age, should still be proactive:
- Testosterone Levels: Monitoring testosterone levels as they can influence bone density.
- Lifestyle Choices: Avoiding smoking and excessive alcohol, which can exacerbate bone loss.
The Intersection of Bone Health and Chronic Illness
Chronic illnesses can have a direct or indirect impact on bone health, necessitating a comprehensive management plan that includes monitoring and maintaining bone integrity.
Chronic Illnesses with Direct Impact on Bones
Conditions such as rheumatoid arthritis or gastrointestinal disorders can directly affect bone health by:
- Inflammation: Leading to increased bone resorption.
- Nutrient Absorption: Impairing the absorption of calcium and other nutrients.
Managing Bone Health with Chronic Illness
To manage bone health when dealing with chronic illness, patients should:
- Follow Treatment Plans: To manage the underlying condition effectively.
- Regular Monitoring: Keeping track of bone density and nutrient levels.
- Collaborative Care: Working with specialists to address all aspects of health, including bone health.
Lifestyle Interventions to Support Bone Health
Adopting a healthy lifestyle is one of the most effective strategies for maintaining bone health. This includes a variety of practices:
Smoking Cessation and Alcohol Moderation
Both smoking and excessive alcohol consumption can have detrimental effects on bone health, so it is recommended to:
- Quit Smoking: Seek support for smoking cessation to improve overall and bone health.
- Limit Alcohol: Keep alcohol consumption within the recommended guidelines.
Weight Management
Being underweight or overweight can negatively impact bone health. Maintaining a healthy weight is beneficial for bones by:
- Reducing Stress on Bones: Excess weight can increase the risk of fractures.
- Improving Hormonal Balance: Optimal weight supports a healthy hormonal environment for bone maintenance.
Environmental and Community Support for Bone Health
The environments in which we live and work can either support or hinder bone health. Communities and workplaces can take action to promote bone health by:
Community Initiatives
- Public Education: Raising awareness about the importance of bone health.
- Recreational Spaces: Providing parks and facilities that encourage physical activity.
Workplace Wellness Programs
Employers can support bone health by:
- Ergonomic Work Environments: Reducing the risk of musculoskeletal disorders.
- Health and Wellness Programs: Offering resources for smoking cessation and weight management.
The Future of Bone Health: Innovations and Research
Ongoing research and technological advancements continue to enhance our understanding and management of bone health. Emerging therapies and diagnostics are paving the way for personalized and effective bone health strategies.
Advances in Bone Health Research
New research focuses on:
- Genetic Markers: Identifying genetic predispositions to bone diseases.
- Novel Therapeutics: Developing medications that target specific pathways in bone metabolism.
The Promise of Technology
Technological innovations such as wearable devices that monitor physical activity and advancements in imaging techniques are contributing to more precise assessments and interventions for bone health.
The Role of Healthcare Providers in Bone Health
Healthcare providers play a pivotal role in the prevention and management of bone-related diseases. Through patient education, regular screenings, and collaborative care, they can help individuals maintain healthy bones throughout their lives.
Collaboration Across Specialties
Bone health often requires the collaboration of primary care physicians, endocrinologists, orthopedists, and other specialists to provide comprehensive care.
Ongoing Patient Education
Providers should continually educate patients on the importance of diet, exercise, and lifestyle choices in maintaining bone health, as well as the risks and benefits of treatments and supplements.
Navigating Bone Health Through Education and Advocacy
Education and advocacy are vital components in the promotion of bone health. Understanding the factors that affect bone health and advocating for better resources and policies can lead to a healthier society.
The Power of Information
Providing accessible and accurate information empowers individuals to make informed decisions about their bone health.
Advocacy for Better Bone Health Policies
Advocating for policies that support research, healthcare access, and community resources can improve bone health outcomes on a larger scale.
Conclusion
As we explore the multifaceted aspects of bone health, it becomes clear that it requires a comprehensive approach. From individual choices to societal factors, each plays a significant role in the development and maintenance of our skeletal framework. By staying informed and proactive, we can all contribute to the foundation of stronger bones for a healthier future. While this article does not contain a conclusion, it is evident that the journey to optimal bone health is ongoing and requires consistent effort and attention.
As we delve deeper into the intricacies of bone health, it becomes increasingly clear that our actions and choices have profound implications for the well-being of our skeletal system. To ensure the vigor and resilience of our bones, concerted efforts must be made not only in our individual health routines but also at the community and policy levels.
The Synergy of Diet and Exercise in Bone Health
The synergistic relationship between diet and exercise plays a pivotal role in achieving and maintaining optimal bone health. A nutrient-dense diet lays the foundation, while physical activity builds upon it to enhance and preserve bone density.
Integrating Bone-Strengthening Activities
To maximize the benefits of exercise for bone health, individuals should aim to integrate a variety of bone-strengthening activities into their routine:
- High-Impact Weight-Bearing Exercises: Such as running, jumping, or plyometric workouts, which are especially beneficial for younger individuals in building bone density.
- Low-Impact Weight-Bearing Exercises: Including walking and elliptical training, suitable for all ages and particularly for those who may not tolerate high-impact activities.
- Muscle-Strengthening Exercises: Utilizing resistance bands, free weights, or bodyweight exercises to apply stress to bones and muscles, thereby stimulating bone growth.
- Balance and Flexibility Workouts: Activities like yoga and tai chi not only enhance balance, reducing the risk of falls, but also promote joint mobility and bone health.
The Influence of Nutritional Choices
Nutritional choices are crucial in supporting bone health. A balanced diet rich in calcium, vitamin D, and other bone-friendly nutrients is essential. Here are some dietary habits that can benefit bone health:
- Diverse and Balanced Diet: Including a variety of food groups to ensure a comprehensive nutrient intake.
- Calcium-Rich Foods: Prioritizing dairy products, leafy greens, and fortified alternatives.
- Vitamin D Sources: Fatty fish, sunlight exposure, and fortified foods to facilitate calcium absorption.
- Adequate Protein: Ensuring sufficient protein intake, which is crucial for bone repair and maintenance.
The Impact of Socioeconomic Factors on Bone Health
Socioeconomic factors, such as access to healthy foods and recreational spaces, can significantly impact an individual’s ability to maintain bone health. Areas with limited resources may see higher rates of bone-related diseases due to these disparities. Addressing these issues requires a multifaceted approach that includes improving access to nutritious foods, providing education on bone health, and investing in community spaces that encourage physical activity.
The Role of Supplements in Bone Health
While a well-rounded diet is the most effective way to receive necessary nutrients, there may be circumstances where dietary supplements can play a supportive role in maintaining bone health:
- Calcium Supplements: For those who cannot meet their calcium needs through diet alone.
- Vitamin D Supplements: Especially for individuals in regions with limited sunlight or those with absorption issues.
- Supplements for Specific Needs: Such as magnesium, vitamin K, or phosphorus for individuals with unique nutritional needs or restrictions.
It is imperative, however, to consult with a healthcare provider before beginning any supplement regimen to ensure appropriate dosing and to avoid potential adverse interactions with other medications.
The Technological Frontier in Bone Health
Technological advancements are opening new avenues for the assessment and management of bone health. Wearable technology can track physical activity levels and provide feedback to encourage movement throughout the day. Additionally, innovations in imaging techniques are allowing for more detailed and earlier detection of bone density changes, potentially leading to more timely interventions.
Emerging Therapies
Research is constantly uncovering new therapeutic targets for bone health. The development of new medications that act on specific pathways in the bone remodeling process holds the promise of more personalized and effective treatments for bone diseases like osteoporosis.
The Importance of Community and Policy in Bone Health
The health of our bones is not solely a personal matter; it is also a community and societal issue. Community initiatives and public policies play a crucial role in promoting bone health across populations.
Community Initiatives:
- Educational Programs: Providing information on nutrition, exercise, and lifestyle choices that support bone health.
- Access to Nutritious Foods: Establishing community gardens and supporting local farmers’ markets to increase the availability of healthy food options.
- Recreational Infrastructure: Developing parks, trails, and community centers that facilitate physical activity for all age groups.
Policy Measures:
- Healthcare Access: Ensuring that all individuals have access to preventative care and screenings for bone health.
- Research Funding: Investing in research to better understand bone health and develop more effective treatments.
- Workplace Health: Encouraging employers to implement wellness programs that support physical activity and healthy lifestyle choices.
The Role of Personal Responsibility and Advocacy
While community and policy initiatives are vital, personal responsibility remains a key element in maintaining bone health. Individuals must take an active role in their health by making informed choices and advocating for themselves and others.
Personal Advocacy:
- Staying Informed: Keeping up-to-date with the latest research and guidelines on bone health.
- Healthcare Communication: Engaging in open dialogue with healthcare providers to create personalized bone health plans.
- Community Involvement: Participating in or leading community efforts to promote bone health and wellness.
Conclusion
Bone health is a vital component of overall well-being that spans the entirety of one’s life. From childhood through old age, the choices we make can significantly influence the strength and integrity of our bones. By understanding and integrating the principles of proper nutrition, regular exercise, and a proactive approach to healthcare, we can build a solid foundation for our skeletal system. Additionally, advancing technologies, community support, and effective policies are essential in creating an environment conducive to optimal bone health. As we continue to evolve in our understanding of bone health, it is crucial that we remain committed to the practices that will ensure our bones remain robust and capable of supporting us through a vibrant and active life.
In closing, this article has outlined the importance of a comprehensive approach to maintaining bone health. It has highlighted the significance of dietary choices, physical activity, genetic factors, and the role of community and policy in shaping our bone health outcomes. By taking personal responsibility and advocating for broader support systems, we can ensure that the foundation of our body—the skeleton—remains strong and resilient, allowing us to lead fulfilling lives.
To all those committed to the journey of maintaining bone health: may you continue to stay informed, engaged, and proactive in your pursuit of a lifetime of strength and vitality.