Intermittent fasting (IF) has become a popular health and wellness trend, not only for weight loss but also for its potential benefits in managing various health conditions, including gastrointestinal (GI) issues. This practice of cycling between periods of fasting and eating can vary in duration and frequency but often includes daily time-restricted feeding or 24-hour fasts several times per week. The impact of intermittent fasting on digestive health is multifaceted, influencing gut microbiota, mucosal integrity, and immune function.
The Gut Health Connection
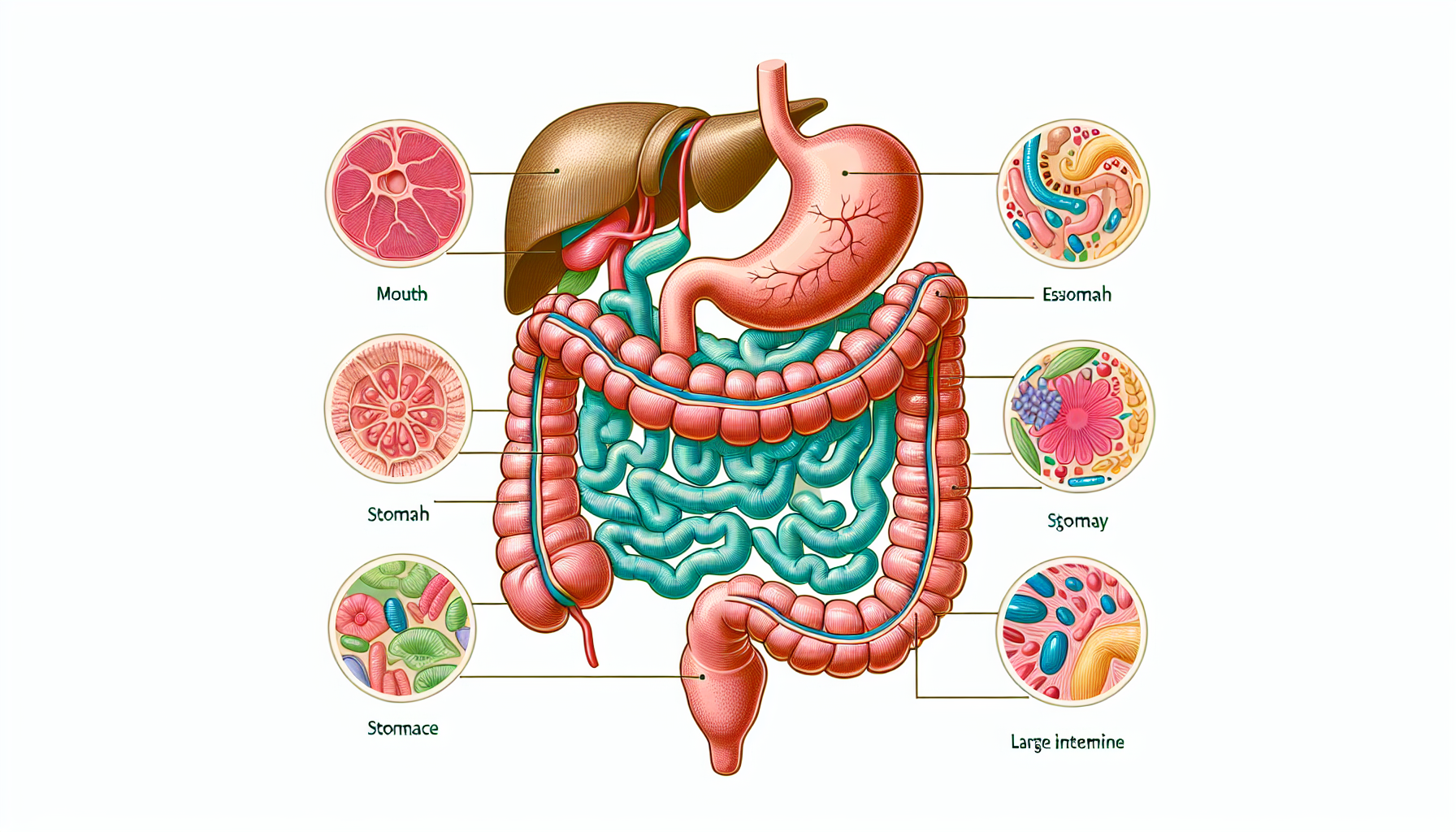
The digestive system is a complex network that plays a crucial role in overall health. Disorders such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), and gastroesophageal reflux disease (GERD) can significantly affect quality of life. Digestive Health is paramount, given its connection to nutrient absorption, immune function, and even mental health through the gut-brain axis.
Fasting and Gut Rest
One advantage of intermittent fasting is that it allows the GI tract to rest. During fasting periods, the digestive system is not burdened with the constant processing of food, which can help reduce inflammation and improve symptoms in individuals with chronic GI conditions. It’s akin to rebooting a system, giving the gut an opportunity to repair and restore.
The Microbiome and Fasting
Intermittent fasting can modify the gut microbiome, the community of microorganisms residing in the intestines. A balanced microbiome is essential for digestive health, and IF has been shown to promote beneficial shifts in microbial populations. For instance, fasting can increase the growth of certain bacteria known for anti-inflammatory properties, potentially offering relief to those with GI disorders.
Immune Regulation
The immune system is intricately linked with gut health, and fasting can modulate immune responses. The reduction in inflammation associated with IF might alleviate symptoms of autoimmune conditions affecting the gut, such as Crohn’s disease. Moreover, IF has been linked to improved immune surveillance, which could protect the gut from pathogenic infections.
Addressing Specific Gastrointestinal Issues with IF
Intermittent fasting’s impact on various GI disorders has been an area of growing interest. Below are some conditions that may be positively affected by IF:
Irritable Bowel Syndrome (IBS)
IF can help in managing IBS by regulating the motility and function of the GI tract, potentially reducing bloating, cramping, and irregular bowel movements.
Inflammatory Bowel Disease (IBD)
The anti-inflammatory effects of fasting can benefit those with IBD, as fasting may help in reducing the frequency and severity of flare-ups.
GERD and Acid Reflux
By limiting food intake to specific windows, IF can decrease the likelihood of acid reflux, a common symptom of GERD.
Nutritional Considerations and Fasting
While intermittent fasting can have potential GI benefits, it’s crucial to maintain a balanced diet during eating periods. Incorporating foods rich in fiber, probiotics, and anti-inflammatory properties is vital. For insights on a healthy diet during IF, explore resources on nutritional tips for restoring gut health and the importance of enzyme diversity in digestive health.
External Resources Supporting IF for GI Health
When considering intermittent fasting for GI issues, it’s essential to review scientific literature and expert guidance. Here are some niche resources that provide in-depth information on the subject:
- An in-depth review of the impact of fasting on the gut microbiome published in a peer-reviewed journal.
- Clinical guidelines on managing IBD with diet, including fasting protocols.
- A detailed analysis of the mechanisms behind fasting and immune system regulation in the context of GI health.
Additional Considerations and Precautions
Intermittent fasting is not suitable for everyone. Individuals with a history of eating disorders, those who are pregnant or breastfeeding, and people with certain medical conditions should consult healthcare professionals before starting an IF regimen. It’s also important to consider the techniques for effective management of chronic gastrointestinal pain and understand the role of plant-based diets in managing GI disorders.
In conclusion, intermittent fasting offers a promising avenue for managing and potentially alleviating symptoms of various gastrointestinal issues. Its ability to provide gut rest, modulate the microbiome, and regulate the immune system makes it a multifaceted approach to digestive health. However, individual responses to fasting can vary, and it should be practiced with consideration of one’s overall health and nutritional needs.
As the understanding of intermittent fasting’s role in GI health continues to evolve, it remains an area ripe for exploration and application. With proper guidance and a mindful approach, IF can be a powerful tool in the quest for digestive wellness and improved quality of life.