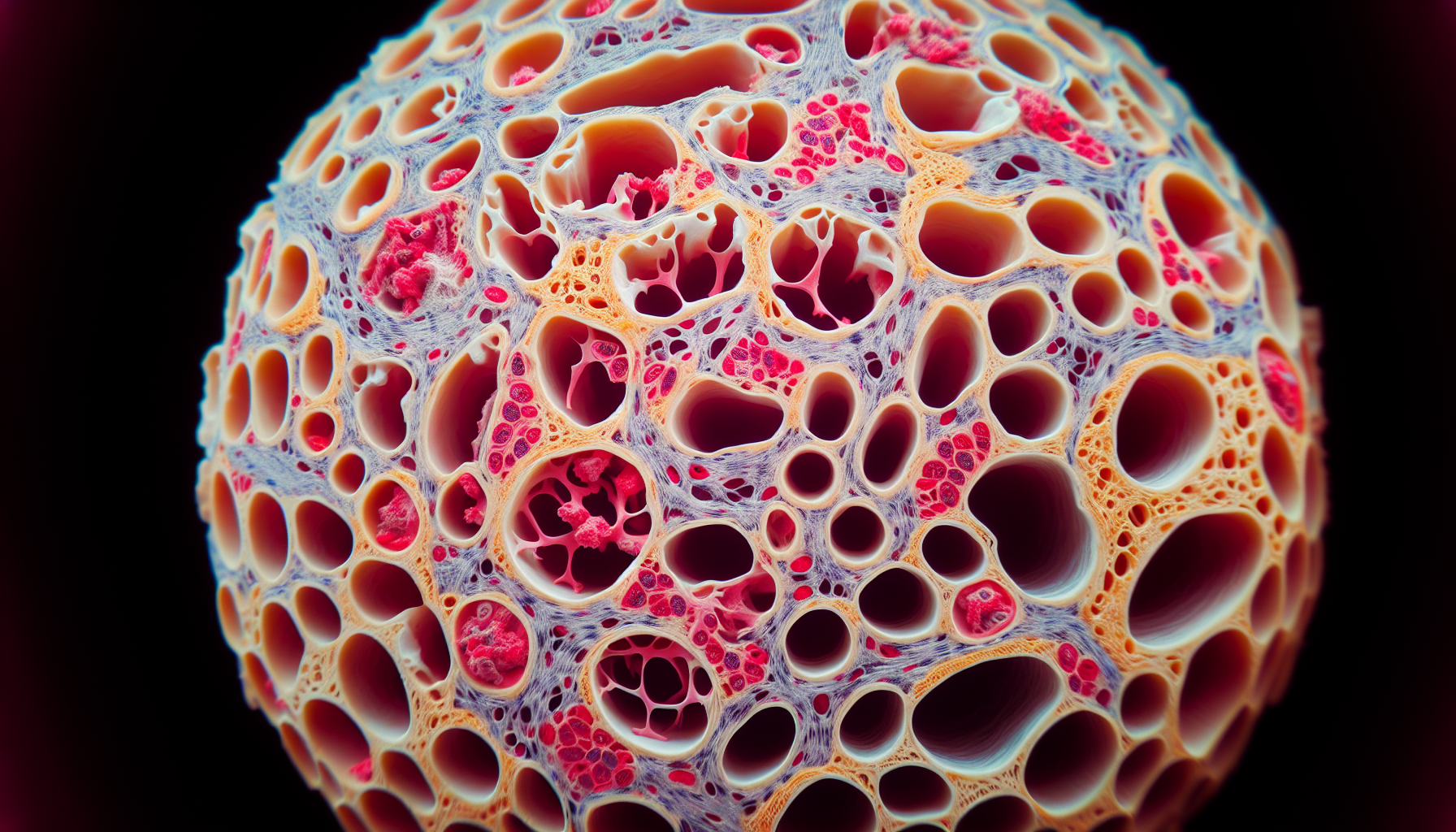
Menopause is a significant phase in a woman’s life marked by the end of menstrual cycles, which typically occurs in the late 40s to early 50s. While menopause is a natural biological process, it comes with a host of changes that can impact a woman’s health in various ways. One of the most profound effects of menopause is on bone mass. The decline in estrogen levels during menopause can lead to a decrease in bone density, increasing the risk of osteoporosis and fractures. This article delves into the intricate relationship between menopause and bone health, providing insights into how women can manage and mitigate these changes.
The Menopause-Bone Mass Connection
Estrogen is integral to maintaining bone density; it helps regulate the balance between bone resorption and formation. During menopause, the ovaries reduce their production of estrogen, leading to an accelerated phase of bone loss. This phase can last for several years post-menopause, with women potentially losing up to 20% of their bone density during this time.
It’s crucial to acknowledge the importance of bone health as it plays a crucial role in overall wellness, providing structure, protecting organs, anchoring muscles, and storing calcium. Reduced bone mass not only increases the risk of fractures but also can severely impact a woman’s quality of life.
Risk Factors for Bone Mass Reduction in Menopause
Several factors can influence the degree of bone loss a woman may experience during menopause, including:
- Genetics: A family history of osteoporosis can increase risk.
- Lifestyle choices: Smoking, excessive alcohol consumption, and a sedentary lifestyle can exacerbate bone loss.
- Nutrition: Inadequate intake of calcium and vitamin D can lead to weaker bones.
- Body size: Women with a smaller body frame tend to have less bone mass to draw from as they age.
Strategies for Maintaining Bone Health During Menopause
While menopause-induced bone loss is inevitable for most women, there are strategies to maintain bone health and reduce the risk of osteoporosis:
Regular Exercise
Physical activity, especially weight-bearing and resistance exercises, can help build and maintain bone density. The impact of physical activity on bone remodeling is significant, as it stimulates bone formation and strengthens muscles, which can protect and support the skeletal structure.
Nutritional Support
A diet rich in calcium and vitamin D is vital for bone health. Postmenopausal women should ensure they’re meeting their daily requirements for these nutrients to support bone maintenance. Bone Health: Nutritional Guidelines for Seniors offers valuable dietary advice tailored to the needs of older adults.
Mind-Body Practices
Mind-body practices such as yoga and tai chi can improve balance, flexibility, and strength, reducing the risk of falls and related fractures. Moreover, they have stress-reducing benefits which may indirectly support bone health. More on this can be found in the article on how to support bone health with mind-body practices.
Medication and Supplements
In some cases, doctors may prescribe medication to slow bone loss. Additionally, supplements such as calcium and vitamin D are often recommended. For more information on this, you can refer to medication & supplements.
Regular Bone Density Screenings
Regular screenings can help detect bone loss early on. The importance of regular bone density screenings cannot be overstated as it is a preventive measure to avoid the complications associated with osteoporosis.
External Resources Supporting Bone Health During Menopause
To further understand and combat the effects of menopause on bone mass, here are some niche resources offering valuable information:
-
International Osteoporosis Foundation: Their resources provide a global perspective on bone health, with specific sections dedicated to women’s health and menopause (Link to IOF).
-
National Osteoporosis Society: This UK-based charity offers in-depth guides on living with osteoporosis, including managing menopause-related bone loss (Link to NOS).
-
The Endocrine Society: They have published research and clinical practice guidelines on the management of menopausal symptoms, including bone health (Link to Endocrine Society).
-
Menopause Society: A comprehensive hub for information regarding menopause, including its impact on bone health (Link to Menopause Society).
-
Nutrition Studies Research Group: Research on the impact of nutrition on bone health during menopause, providing evidence-based dietary recommendations (Link to Nutrition Studies).
These resources offer detailed insights and evidence-based recommendations that can help women navigate through menopause with a focus on maintaining bone mass and overall health.
Conclusion
Menopause is a natural transition that can have significant effects on bone mass due to the decline in estrogen levels. By understanding these changes and implementing strategies such as regular exercise, proper nutrition, mind-body practices, appropriate use of medication and supplements, and regular bone density screenings, women can proactively manage their bone health during and after menopause. It’s essential to utilize both professional guidance and the wealth of information available through specialized resources to support bone health during this critical period of a woman’s life.