Heart disease remains the leading cause of mortality for women around the globe, particularly for those who have transitioned into postmenopause. The hormonal shifts that occur during this stage of life can lead to cardiovascular changes, making an understanding of the risks and preventive measures crucial for maintaining heart health. This comprehensive exploration delves into the intricacies of heart disease in postmenopausal women, offering insights for prevention, management, and the importance of a holistic approach to health.
Hormonal Changes and Cardiovascular Risk
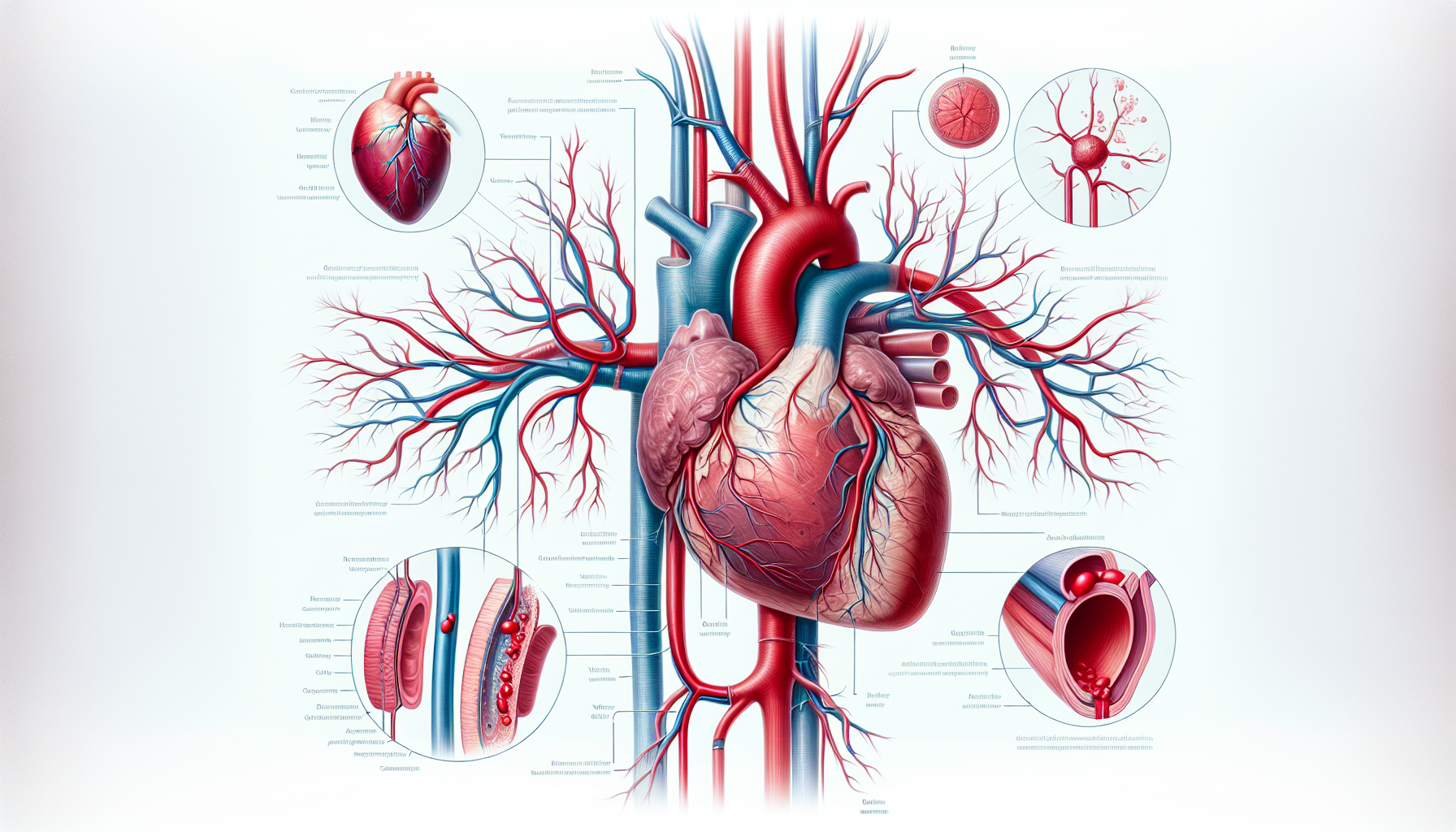
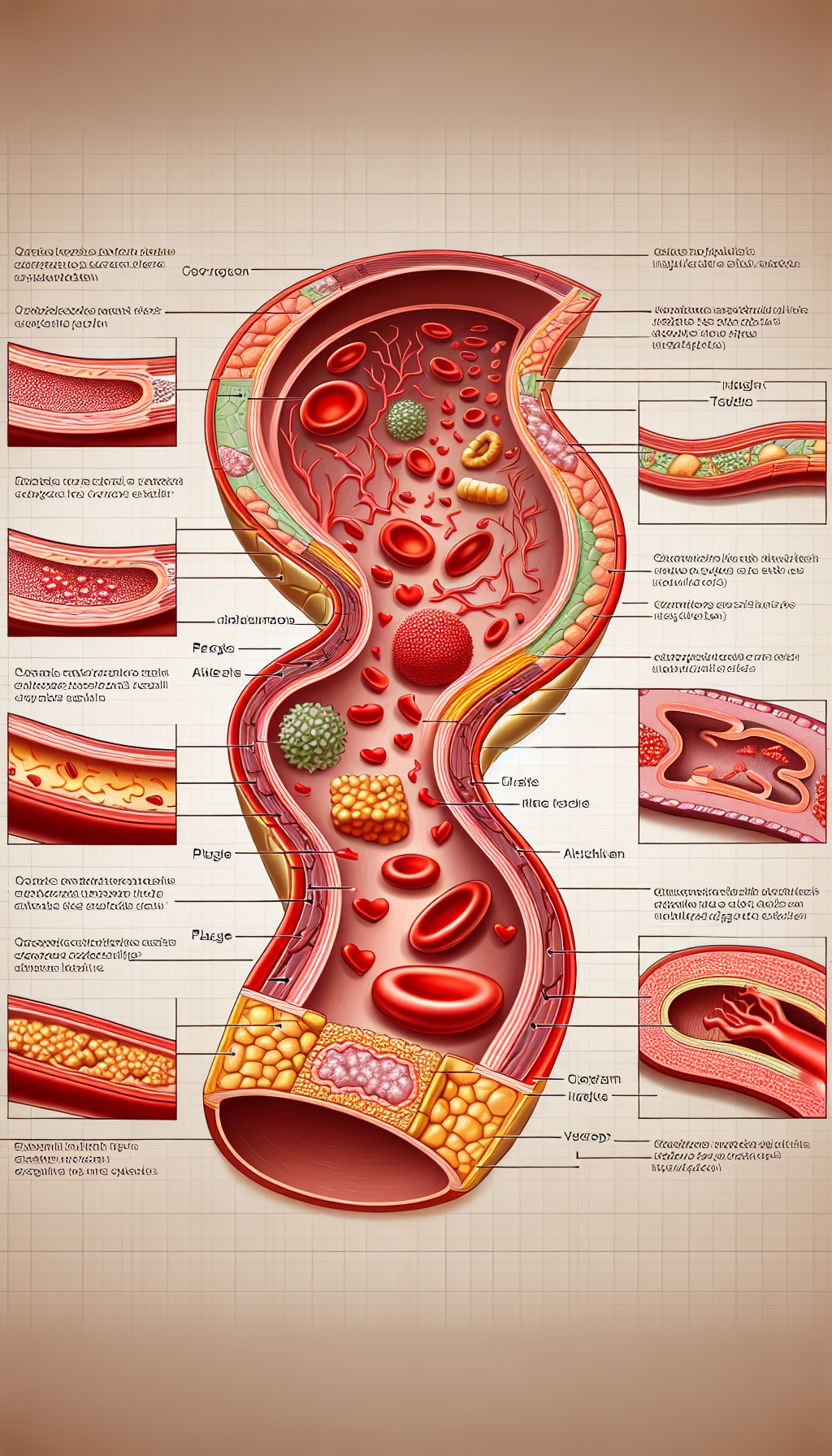
The cessation of menstruation marks the onset of menopause, typically occurring between the ages of 45 and 55. This period brings about a decline in the production of estrogen and progesterone, hormones that are thought to offer some cardioprotective effects. The drop in estrogen levels is particularly significant, as it can contribute to the development of atherosclerosis—a condition characterized by the hardening and narrowing of the arteries, which can lead to heart attacks and strokes.
Estrogen and Heart Health
Estrogen is believed to have a positive effect on the inner layer of artery walls, helping to keep blood vessels flexible and allowing them to relax and expand to accommodate blood flow. Additionally, estrogen plays a role in maintaining a favorable lipid profile, which includes higher levels of "good" HDL cholesterol and lower levels of "bad" LDL cholesterol. The absence of these protective effects postmenopause can lead to an increased risk of coronary artery disease.
Blood Pressure and Menopause
Blood pressure can also rise during postmenopause, further escalating the likelihood of heart disease. The exact mechanisms behind this increase are not fully understood, but they may relate to changes in body composition, such as increased abdominal fat, and alterations in vascular health.
Strategies for Heart Disease Prevention in Postmenopausal Women
To mitigate these risks, postmenopausal women are encouraged to adopt a heart-healthy lifestyle. This includes engaging in regular physical activity, eating a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats, and maintaining a healthy weight. Additionally, managing stress, avoiding smoking, and limiting alcohol intake are important lifestyle modifications that can contribute to cardiovascular health.
For more detailed strategies on enhancing cardiovascular well-being, visit Cardiovascular Health on the Avix Health website.
Importance of Regular Health Screenings
Regular health screenings become increasingly important as women transition into postmenopause. Monitoring blood pressure, cholesterol levels, and blood sugar can help detect early signs of heart disease, allowing for timely intervention. Regular echocardiograms, as highlighted in "The Significance of Regular Echocardiograms in Heart Disease Management," are also vital for tracking heart function and structure.
Exercise and Heart Health
Exercise is a cornerstone of heart disease prevention. High-Intensity Interval Training (HIIT), for instance, has been shown to improve cardiovascular health and can be an effective component of a fitness regimen for postmenopausal women. To learn more, read "Maximizing Cardiac Health with High-Intensity Interval Training."
Nutritional Supplements
Nutritional supplements can also play a role in maintaining heart health. Coenzyme Q10, for example, has been linked to improved heart function and may help reduce the risk of heart disease. For further information, consider "The Relationship Between Coenzyme Q10 and Heart Health Maintenance."
The Role of Medications
Postmenopausal women may be prescribed medications to manage risk factors for heart disease, such as statins for high cholesterol or antihypertensive drugs for high blood pressure. While these medications can be life-saving, it is important to be aware of potential cardiovascular risks associated with long-term use. Explore these considerations further in "Cardiovascular Disease Risks Associated with Long-term Medications."
External Supportive Resources
Several niche resources provide in-depth information supporting the points made above:
- The American Heart Association offers detailed guidance on heart health for women, with a focus on postmenopausal concerns.
- The National Institutes of Health has a page dedicated to menopause and heart disease, which discusses how menopause can change your risk for heart disease.
- The North American Menopause Society provides resources about women’s health and menopause, including the impacts on cardiovascular health.
- Hormone Health Network, from the Endocrine Society, offers a comprehensive look at menopause and cardiovascular disease.
- The British Heart Foundation presents insights into how your heart is affected by the menopause.
The Integration of Mental and Overall Health
Mental health can significantly impact heart health, with stress, anxiety, and depression all having the potential to affect cardiovascular well-being. Adopting a holistic approach that includes mindfulness, meditation, and therapy can be beneficial. The interconnectedness of mental and heart health is further explored in "Linking Mental Health and Heart Health for a Holistic Approach."
Conclusion
Heart disease in postmenopausal women presents unique challenges that require a multifaceted approach to prevention and management. By understanding the risks, engaging in preventive strategies, and utilizing regular health screenings, postmenopausal women can take proactive steps towards maintaining their heart health.
It is essential for women to have conversations with their healthcare providers about heart health postmenopause. Together, they can develop a personalized plan that addresses individual risks and lifestyle factors, ensuring the best possible outcomes for cardiovascular health and overall well-being.
Navigating the journey of postmenopause does not have to be a path walked alone. With informed choices, supportive healthcare, and a community of resources, women can thrive during this chapter of their lives with strong, healthy hearts.